Medication Timing Checker
Medication Timing Checker
Find out if the timing of your medications matters for effectiveness and side effects.
Key Takeaways
For timing-sensitive medications:
- Set reminders with alarms or pill organizers
- Anchor doses to daily habits (e.g., after brushing teeth)
- Keep a log of when you take medications
- Always consult your pharmacist or doctor before changing medication timing
What if taking your pill five minutes earlier-or later-could mean the difference between feeling fine and ending up in the hospital? It sounds extreme, but for many medications, timing isn’t just a suggestion. It’s a safety rule.
Why Your Body Has a Clock
Your body doesn’t just wake up and go to sleep-it runs on a 24-hour rhythm called the circadian clock. This internal timer controls everything from your body temperature and hormone levels to how your liver breaks down drugs. When you take a medication, your body doesn’t treat it the same way at 8 a.m. as it does at 8 p.m. Liver enzymes that metabolize drugs can be twice as active at night. Blood pressure naturally dips during sleep. Cholesterol production peaks in the early hours. And if you’re taking medication that interacts with any of these rhythms, getting the timing wrong can make side effects worse-or make the drug less effective.When Timing Matters Most
Not all meds need perfect timing. A missed dose of a statin by an hour? Probably fine. But for others, even a 15-minute delay can cause trouble.- Insulin: If you take rapid-acting insulin too early before a meal, your blood sugar can crash. Too late, and it spikes. Studies show mistimed insulin leads to hypoglycemia in up to 22% of cases.
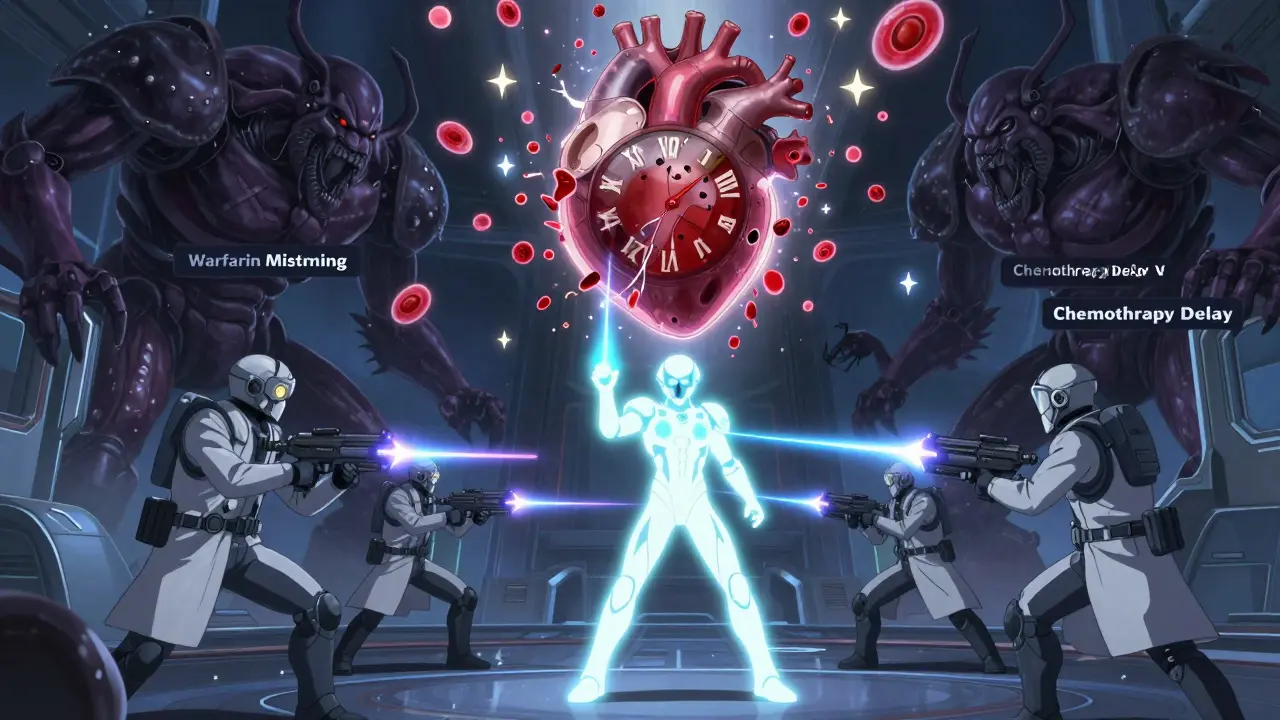
- Anticoagulants (like warfarin): These thin your blood. If you take them at inconsistent times, your INR levels swing, increasing bleeding risk by as much as 37%.
- Chemotherapy drugs: Timing matters because cancer cells divide at certain times. Deviating from the schedule by more than 30 minutes can cut effectiveness by 15-20%.
- Statins: These lower cholesterol, but they work best when taken at night. That’s when your liver makes the most cholesterol. Evening dosing can improve LDL reduction by 15-20% compared to morning doses.
- ACE inhibitors for high blood pressure: Taking these at bedtime, not in the morning, reduces cardiovascular events by nearly 30% in people with hypertension. Nighttime dosing helps control the morning blood pressure surge, when heart attacks and strokes are most common.
These aren’t opinions. They’re backed by clinical trials. The MAPEC study, which tracked over 2,000 hypertensive patients for six years, found that bedtime dosing of blood pressure meds cut heart attacks, strokes, and heart failure by almost a third.
When Timing Doesn’t Matter (Much)
You don’t need to set an alarm for every pill. Some drugs are forgiving. For example:- Hydrochlorothiazide (a water pill): A 12-hour window won’t hurt. It’s designed for steady, long-term use.
- Most antibiotics: As long as you take them every 8 or 12 hours, a 30-minute variation won’t break the cycle.
- Many pain relievers: Ibuprofen or acetaminophen can be taken within a few hours of the target time without major risk.
The key is knowing which category your meds fall into. If you’re unsure, ask your pharmacist. Don’t assume all pills are the same.

Why Hospitals Get It Right (And You Might Not)
In hospitals, nurses follow strict protocols. They use barcode scanners, timed alerts, and double-checks. Even then, timing errors happen in nearly half of IV medication administrations. Outside the hospital, things get messy.Patients juggle work, kids, travel, and sleep. A 7 a.m. dose becomes 11 a.m. because you overslept. A 10 p.m. pill gets skipped because you’re out for dinner. A 2021 survey of 1,200 people found that 68% of those on chronotherapy-sensitive meds (like statins or blood pressure drugs) couldn’t stick to a consistent schedule. The biggest reason? Low health literacy. People didn’t understand why timing mattered.
Another big problem? Interruptions. A 2008 JAMA study showed that every time a nurse gets interrupted during a med pass, the error rate climbs. Five interruptions? The chance of a timing mistake jumps from 39% to 61%. At home, distractions are even worse-phone calls, doorbells, kids crying. One nurse on Reddit wrote: “We’re lucky to get within 30 minutes of scheduled times.”
What You Can Do
You don’t need a hospital-grade system to get timing right. Here’s how to make it easier:- Ask your pharmacist: “Is timing important for this drug?” Don’t assume. Ask for a simple label: “Take at bedtime,” “Take with food,” “Take at the same time daily.”
- Use a pill organizer with alarms: Simple phone alarms or smart pill dispensers (like MedMinder) can remind you. Set two: one for the time, one for 15 minutes later as a backup.
- Anchor to daily habits: Take your pill after brushing your teeth, with breakfast, or right before bed. Linking it to something you already do makes it stick.
- Keep a log: For high-risk meds (like warfarin or insulin), write down when you took it. Even a note on your phone helps.
- Check for interactions: Some meds (like grapefruit juice or St. John’s Wort) change how your body processes drugs. Timing won’t help if the interaction is already messing with your system.
The Future: Personalized Timing
Scientists are now looking beyond “take at night” to “take at 11:47 p.m. because of your genes.” The ChronoGene study, due to finish in late 2024, is testing whether genetic variations in your body’s clock genes affect when your meds work best. One person might absorb a drug fastest at 8 p.m., another at 1 a.m. That’s the next frontier: personalized chronotherapy.Already, the FDA is requiring drug makers to include circadian data in new drug applications. In 2022, they reviewed 17 such submissions-up from just 3 in 2018. Epic’s new ChronoCare module now flags timing risks in electronic health records. This isn’t science fiction. It’s coming to your pharmacy.
Bottom Line
Timing isn’t about perfection. It’s about awareness. For some meds, it’s life-changing. For others, it’s just good practice. The goal isn’t to stress over every minute-it’s to know which drugs need your attention and why. If you’re on blood pressure meds, statins, insulin, or blood thinners, get clear on your timing. Talk to your doctor. Use a reminder. Log it. Your body’s clock is already working. You just need to work with it.Does it really matter what time I take my medication?
Yes-for certain medications. Drugs like insulin, blood thinners, statins, and some blood pressure meds have timing rules based on how your body processes them. For others, like pain relievers or most antibiotics, being off by an hour usually doesn’t matter. The key is knowing which ones need precision.
Can taking a pill at the wrong time cause serious side effects?
Absolutely. Taking insulin too early can cause dangerous low blood sugar. Taking warfarin inconsistently can lead to bleeding or clots. Chemotherapy timing affects how well it kills cancer cells. Studies show mistimed doses increase major side effects by up to 37% for anticoagulants and 22% for insulin. While most timing errors aren’t life-threatening, the risk is real for high-risk meds.
Why are statins better taken at night?
Your liver makes most of its cholesterol overnight. Statins block an enzyme involved in that process. Taking them at night lines up with your body’s natural production cycle, making them 15-20% more effective at lowering LDL (bad) cholesterol than taking them in the morning.
I’m on multiple medications. How do I keep track of timing?
Use a pill organizer with alarms, or a smartphone app like Medisafe or MyTherapy. Ask your pharmacist to group meds by timing: “morning,” “evening,” “with food.” Write down each med’s timing requirement on a sticky note and stick it to your pill box. If you’re overwhelmed, schedule a med review with your pharmacist-they can help simplify your schedule.
Are there apps or tools that help with medication timing?
Yes. Apps like Medisafe, MyTherapy, and CareClinic send reminders and track adherence. Smart pill dispensers like MedMinder or Hero automatically release pills at set times and alert caregivers if a dose is missed. Hospitals use barcode systems to reduce errors-home versions are now affordable and easy to use.
Can I change my medication timing on my own?
Only if your doctor or pharmacist says it’s safe. For some meds, like blood pressure drugs, switching from morning to bedtime can improve results. For others, like seizure meds or insulin, changing timing without guidance can be dangerous. Never adjust timing without consulting your provider.
Why do hospitals have stricter timing rules than home care?
Hospitals use technology (barcodes, electronic records), trained staff, and protocols to reduce errors. At home, distractions are higher, and people often don’t know which meds need precision. Hospitals also track outcomes closely-timing errors are linked to patient harm, so they’re treated as safety issues. Outside hospitals, it’s often left to the patient to manage.
Is chronotherapy widely used by doctors?
It’s growing, but still underused. Academic hospitals are more likely to follow chronotherapy guidelines-42% do-compared to only 14% of community hospitals. Many primary care doctors aren’t trained in it. But with new FDA guidance and electronic health record updates, it’s becoming part of standard practice. If your doctor doesn’t mention timing, ask them.


Natasha Sandra
December 25, 2025 AT 01:54Sumler Luu
December 26, 2025 AT 07:59sakshi nagpal
December 27, 2025 AT 13:39Sandeep Jain
December 28, 2025 AT 22:23roger dalomba
December 30, 2025 AT 00:14Brittany Fuhs
December 31, 2025 AT 06:26Sophia Daniels
January 2, 2026 AT 05:22Fabio Raphael
January 3, 2026 AT 10:12Amy Lesleighter (Wales)
January 4, 2026 AT 19:14Becky Baker
January 5, 2026 AT 23:12Rajni Jain
January 7, 2026 AT 14:45Nikki Brown
January 9, 2026 AT 11:35Peter sullen
January 10, 2026 AT 15:04