When you get an injection, you expect it to be safe. You don’t think about the air around it, the gloves the technician wore, or how many times the room was cleaned before that vial was filled. But behind every sterile injectable - whether it’s insulin, chemotherapy, or a COVID vaccine - is a highly controlled, meticulously engineered process designed to keep out even a single microbe. One microorganism in a syringe can cause sepsis. One particle can trigger a fatal reaction. That’s why sterile manufacturing for injectables isn’t just about cleanliness. It’s about physics, chemistry, and precision engineering operating at the edge of what’s possible.
Why Sterility Isn’t Optional
Oral pills pass through the stomach, where acid and enzymes kill most invaders. Injectables don’t have that luxury. They go straight into your bloodstream. No filters. No defenses. That’s why the FDA and WHO set the bar at a sterility assurance level (SAL) of 10^-6 - meaning, for every million doses made, no more than one might be contaminated. That’s not a suggestion. It’s a legal requirement.
The stakes became terrifyingly clear in 2012. The New England Compounding Center distributed tainted steroid injections. Fungi got into the vials. 751 people got sick. 64 died. The CDC called it the worst public health disaster in U.S. history tied to a pharmaceutical product. That outbreak didn’t happen because someone was lazy. It happened because the systems weren’t built to handle the risk. Today, every sterile facility is built to prevent that exact scenario.
Two Paths to Sterility: Terminal vs. Aseptic
There are only two ways to make sterile injectables: terminal sterilization and aseptic processing. And they’re as different as baking a cake versus assembling a watch in a dust-free room.
Terminal sterilization means you fill the vial, seal it, then blast it with steam at 121°C for 15-20 minutes. Or you zap it with gamma radiation. This kills everything. It’s simple. Reliable. And FDA-preferred. But here’s the catch: only 30-40% of injectables can survive this. Biologics - like monoclonal antibodies, gene therapies, or protein-based drugs - are too delicate. Heat or radiation breaks them down. So for those, you need aseptic processing.
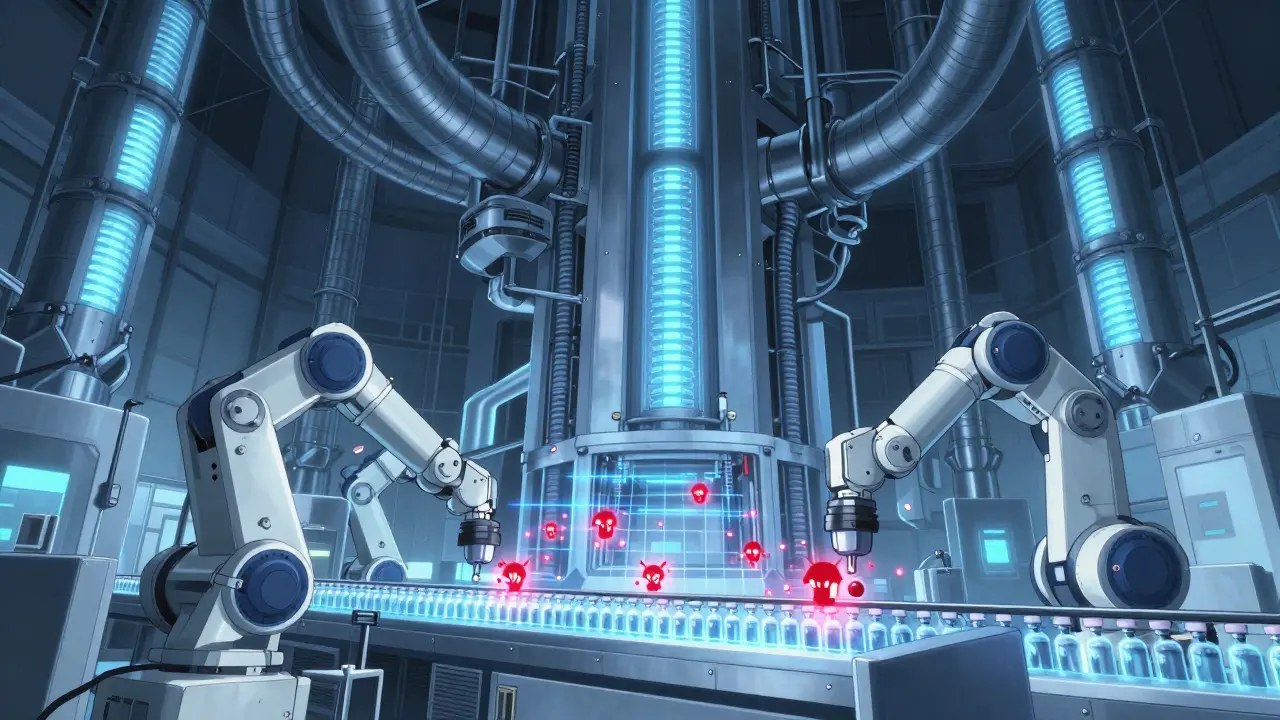
Aseptic processing is where things get intense. No heat. No radiation. Instead, you create a bubble of perfect air. Workers in full-body suits move through layers of cleanrooms - starting at ISO 8 (like a hospital operating room), then moving to ISO 5 (cleaner than a cleanroom in a semiconductor plant). The filling area? ISO 5. That means fewer than 3,520 particles the size of a bacterium per cubic meter of air. For comparison, a typical city street has 35 million particles per cubic meter.
The Cleanroom: A Machine That Breathes
Think of a cleanroom like a living thing. It doesn’t just sit there. It breathes, sweats, and watches itself.
Every hour, the air in an ISO 5 filling room is replaced 20 to 60 times. That’s not a typo. Sixty air changes per hour. Each one filtered through HEPA filters that catch 99.97% of particles down to 0.3 microns. The pressure? 10-15 Pascals higher than the next room. That keeps contaminated air from creeping in. Temperature? 20-24°C. Humidity? 45-55%. Too dry, and static pulls dust. Too wet, and microbes grow.
Water isn’t just purified - it’s Water for Injection (WFI). It’s distilled, filtered, and tested to have less than 0.25 endotoxin units per milliliter. That’s stricter than drinking water standards by 1,000 times. Glass vials? They’re baked at 250°C for 30 minutes to burn off pyrogens - fever-causing toxins left behind by dead bacteria.
Isolators vs. RABS: The Tech Battle
Inside the cleanroom, you’ve got two main systems: RABS (Restricted Access Barrier Systems) and isolators.
RABS are like sealed gloveboxes with open fronts. Workers reach in through gloves to fill vials. They’re cheaper, easier to maintain, and still widely used. But they’re not foolproof. In 2023, a major pharma company had three media fill failures because of tiny holes in their gloves. Each failure cost $450,000 in lost batches.
Isolators are fully enclosed. No human hands enter. Everything moves through airlocks. Robots handle the vials. These systems reduce contamination risk by 100 to 1,000 times compared to RABS. But they cost 40% more to install. And if the automation breaks? You’re stuck.
The debate rages. Renpharm claims isolators hit 0.01 CFU/m³ in air. RABS proponents say properly run RABS can hit the same. The Parenteral Drug Association says both can work - but only if you train people like astronauts.
Media Fills: The Simulation That Saves Lives
Before a sterile line runs a single real dose, it must pass a media fill. This is the ultimate test.
You fill vials with nutrient broth instead of medicine. Then you incubate them for 14 days. If any grow bacteria? The whole process fails. The FDA says a media fill failure rate above 0.1% means your system is broken. That’s one bad vial in every 1,000 tries.
Each simulation runs 5,000 to 10,000 units. That’s not a guess. It’s science. You simulate every possible failure: door opening, equipment jam, glove tear. You do it twice a year. And you document every second.
A survey of 45 sterile facilities found 68% had at least one sterility test failure each year. Each one cost an average of $1.2 million. That’s why companies now use continuous monitoring - sensors that track particles and microbes in real time. Lonza’s facility in Switzerland cut deviations by 45% and sped up batch releases by 30% after installing them.
The Hidden Costs: Training, Testing, and Tech
Setting up a sterile manufacturing line isn’t like buying a new machine. It’s like building a hospital inside a lab.
Minimum investment? $50-100 million for a small facility. That’s for equipment, cleanrooms, validation, and compliance. Personnel? Each worker needs 40-80 hours of aseptic training. And they must requalify every six months. One slip-up - a glove tear, a sneeze near the fill line - can shut down production for weeks.
Documentation? One batch run generates 250-300 pages of records. Fifteen percent of those pages are dedicated to sterility proof: air samples, temperature logs, media fill results. If you can’t prove you followed every step? The FDA shuts you down.
And it’s getting harder. The EU’s revised Annex 1 (2022) demands continuous monitoring - no more weekly checks. The FDA’s 2023 guidance pushes for real-time data analytics and AI-driven inspections. Facilities that don’t upgrade by 2025 risk losing their license.
Where the Industry Is Headed
The sterile injectables market hit $225 billion in 2023. It’s growing at 8.2% a year. Why? Because more drugs - especially biologics - can’t be taken orally. Over 40% of new drugs approved in 2023 required sterile delivery.
Automation is exploding. Robotic filling systems are projected to grow 40% by 2027. Rapid microbiological methods are cutting test times from 14 days to 24 hours. Digital twins - virtual replicas of production lines - are being used to simulate failures before they happen.
But the biggest shift? The move to closed systems. In 2023, 65% of new sterile facilities used fully closed processing. No open vials. No human access. Just automated transfer from mixing to filling to inspection. It’s expensive. But it cuts contamination risk by over 80%.
And the pressure isn’t slowing. The FDA plans to reduce sterile manufacturing deficiencies by 25% by 2026 using AI tools. That means every facility will soon be under constant digital watch.
Final Reality Check
Sterile manufacturing for injectables isn’t glamorous. It’s not talked about. But it’s the invisible shield between you and a deadly infection. Every vial you receive has passed through a gauntlet of engineering, testing, and human discipline.
The systems are expensive. The rules are brutal. The margin for error is zero. And yet, it works. Over 99.9999% of injectables are safe. That’s not luck. It’s science, rigor, and relentless attention to detail - all hidden behind a sterile door, behind a cleanroom, behind a glove, behind a sensor, behind a data point.
If you get an injection today, you’re not just getting medicine. You’re getting a miracle of engineering - one that refuses to let even one microbe slip through.
What’s the difference between terminal sterilization and aseptic processing?
Terminal sterilization kills microbes after the product is sealed, using heat or radiation. It’s reliable but only works for about 30-40% of injectables - mainly those that can handle high temperatures. Aseptic processing keeps everything sterile from start to finish without heat. It’s used for delicate drugs like biologics but requires extreme environmental controls, like ISO 5 cleanrooms and robotic handling. Aseptic is more complex and expensive, but it’s the only option for many modern medicines.
Why do sterile manufacturing facilities need ISO 5 cleanrooms?
ISO 5 is the cleanest classification for aseptic filling. It allows no more than 3,520 particles larger than 0.5 microns per cubic meter of air. That’s about 1,000 times cleaner than a hospital operating room. Since injectables enter the bloodstream directly, even a single particle or microbe can cause serious infection. ISO 5 cleanrooms, with unidirectional airflow and HEPA filtration, create a bubble of near-perfect air to prevent contamination during the most vulnerable step: filling.
What is a media fill, and why is it required?
A media fill is a simulated filling process where sterile broth - not medicine - is put into vials using the exact same equipment and procedures as real production. The vials are then incubated for 14 days to see if any microbes grow. If even one vial shows contamination, the entire process fails. Media fills prove that the system can maintain sterility under real operating conditions. The FDA requires them to be done twice a year, with 5,000-10,000 units per test, to validate that the line won’t contaminate actual products.
How do regulators check if a sterile facility is compliant?
Regulators like the FDA and EMA inspect facilities for documentation, environmental monitoring data, media fill results, personnel training logs, and equipment validation records. They also take air and surface samples on-site. In 2022, 68% of sterile manufacturing deficiencies were due to aseptic technique failures - like improper gowning or uncontrolled movements. The FDA’s 2023 Form 483 reports show that 37% of inspections cited inadequate environmental monitoring, and 28% cited media fill failures. Facilities that don’t meet continuous monitoring and real-time data standards now risk shutdown.
What’s the biggest challenge in sterile manufacturing today?
The biggest challenge is keeping up with regulatory changes while managing cost and complexity. The EU’s Annex 1 revision in 2022 and the FDA’s 2023 guidance require continuous monitoring, real-time data, and AI-driven risk analysis. Many older facilities can’t afford the $15-25 million upgrades needed. Human error remains a top risk - glove tears, improper gowning, and training gaps still cause most failures. The industry is shifting toward automation and closed systems, but retrofitting old lines is slow. The pressure to produce more biologics - which demand aseptic processing - only makes it harder.

Alex Ogle
February 9, 2026 AT 18:25It’s wild to think about how much goes into something so simple. You get a shot, it’s over in seconds. But behind that? A whole universe of air filtration, robotic arms, and people in bunny suits moving like they’re in a sci-fi movie. I used to think ‘sterile’ just meant ‘clean.’ Turns out, it’s like trying to build a snowman in a hurricane and making sure not a single snowflake melts before you finish. The fact that this works 99.9999% of the time is insane. We take it for granted like electricity or running water. But if this system glitches? It’s not a power outage. It’s a death sentence.
Brandon Osborne
February 10, 2026 AT 02:34Someone needs to hold these pharma companies accountable. This whole system is a money machine. They charge $20,000 for a single dose of a biologic because ‘sterile manufacturing is expensive’ - but how much of that is profit? The 2012 outbreak? That was a company cutting corners. And now? They’re just charging more to ‘fix’ what they broke. They don’t want automation because robots don’t unionize. They want humans in bunny suits because humans are cheaper to replace. Wake up. This isn’t science - it’s corporate theater.
Marie Fontaine
February 11, 2026 AT 06:32OMG this is so cool!! 😍 I had no idea about media fills - like, you fill vials with broth and just WAIT? That’s wild. And the ISO 5 cleanroom? 3,520 particles?? I live in a city where my phone picks up 10x that many dust particles just sitting on my desk. 🤯 So many people don’t realize how much science is hiding in plain sight. Kudos to everyone in those rooms - you’re unsung heroes. 🙌
Ken Cooper
February 12, 2026 AT 01:35man i had no idea water for injection was that strict like its not even like purified water its like… witchcraft water? and the glass vials baked at 250c?? why do they even use glass?? why not like… plastic that’s already sterile?? also why do they need 60 air changes per hour?? cant they just like… pump in air from mars??
MANI V
February 13, 2026 AT 02:40This is why the West is failing. You spend $100 million to make one vial of medicine while countries like India and China produce life-saving vaccines for pennies. The obsession with perfection is not purity - it’s arrogance. You want to save lives? Stop over-engineering. Stop the fearmongering. Sterility is a myth. Your body is not a lab. It survives bacteria daily. This system isn’t protecting you - it’s protecting profits.
Random Guy
February 13, 2026 AT 06:50So let me get this straight… we spend billions to keep out ONE microbe… and then we give people a shot that’s basically a 50/50 chance of giving them cancer? 😂
Ryan Vargas
February 15, 2026 AT 01:05The real question isn’t whether sterile manufacturing works - it’s whether we’re being told the whole truth. The SAL of 10^-6? A mathematical abstraction. Real-world contamination is never measured at the source - only after the fact. What if the entire system is designed to create the illusion of safety? What if the sensors, the cleanrooms, the media fills - they’re all performative? We’ve turned medicine into a religion. And like all religions, it demands blind faith. The microbe isn’t the enemy. The system is.
Tasha Lake
February 15, 2026 AT 13:16Just to clarify - when you say ISO 5, that’s Class 100 per Fed Std 209E, right? And the unidirectional laminar airflow is critical for particle displacement, especially at fill lines where turbulence can cause micro-contamination. The HEPA filters are rated to EN 1822 H13, capturing ≥99.95% of 0.3 µm particles. And WFI? It’s not just distilled - it’s passed through reverse osmosis, deionization, and ultrafiltration with a 10 kDa cutoff to remove endotoxins. The validation protocols follow USP <1207> and ICH Q7. It’s insane how precise this all is - and yet, human error still causes 70% of failures. Training is everything.
Sam Dickison
February 16, 2026 AT 17:54Real talk - I work in a sterile facility. The gloves? They’re the worst. One tear and you’re out for 48 hours. We do media fills every 6 months - 10k units. Last time, we had one positive. Turned out someone sneezed into their sleeve during gowning. No one saw it. No one knew. We shut down for two weeks. Cost us $2M. But we fixed it. Now we have real-time airflow sensors and AI that flags movement patterns. If you twitch too fast? The system pauses. It’s wild. But it works. And yeah - it’s expensive. But it’s not optional. Not anymore.
John McDonald
February 18, 2026 AT 11:22Love this breakdown. One thing I’d add - the shift to closed systems isn’t just about contamination. It’s about scalability. Biologics are the future. You can’t hand-fill 500,000 vials a day with RABS. Robots don’t get tired. They don’t sneeze. They don’t need breaks. And with digital twins, we can simulate 10,000 failure scenarios before the first vial’s even filled. The future isn’t cleanrooms with humans. It’s fully automated, AI-monitored, self-correcting production lines. We’re not just making medicine anymore. We’re building living systems.
Andy Cortez
February 20, 2026 AT 10:36so uhh… if you’re telling me they bake glass vials at 250c… then why do they still use glass?? like… what if… we just… made the medicine in the syringe??
Andrew Jackson
February 22, 2026 AT 00:31This nation has lost its way. We have surrendered our health to a technocratic elite who demand billion-dollar cleanrooms to inject people with substances they refuse to explain. The FDA, the WHO - they are not guardians of public health. They are gatekeepers of a global pharmaceutical cartel. The 10^-6 standard? A smokescreen. The truth? The system is designed not to prevent contamination - but to justify perpetual dependence on expensive, proprietary, unaffordable medicine. This is not science. This is control.
Joseph Charles Colin
February 22, 2026 AT 15:34Just to clarify the terminal vs aseptic point - terminal sterilization is only applicable to small molecules with thermal stability. Most biologics (mAbs, vaccines, gene therapies) are thermolabile. Aseptic processing is non-negotiable here. The ISO 5 environment isn’t just about particle count - it’s about viable particle control. That’s why we monitor for CFU, not just particles. And the media fill? It’s not just a test. It’s a process qualification. The FDA requires it under 21 CFR 211.113. You can’t skip it. And yes - isolators are superior. But RABS can be validated to the same level with rigorous training and dynamic monitoring. The key isn’t the hardware. It’s the culture.