When you pick up a prescription, you might assume the pharmacist will always give you the cheapest version of your medicine. But that’s not true everywhere. In some states, pharmacists must swap your brand-name drug for a generic. In others, they can only do it if they think it’s okay-and even then, they might need your permission. These differences aren’t just paperwork. They affect how much you pay, whether you stick with your treatment, and even how often you end up back in the doctor’s office.
What’s the Real Difference Between Mandatory and Permissive Substitution?
Mandatory substitution means the law forces pharmacists to give you the generic version unless your doctor specifically says no. Permissive substitution means the pharmacist can choose to swap it, but isn’t required to. Sounds simple, right? But the details matter more than you think. In 19 states-including Alabama, Arizona, Connecticut, and West Virginia-pharmacists have no choice. If a generic is available, FDA-approved, and cheaper, they have to dispense it. No asking. No waiting. Just swap and go. In the other 31 states, the decision is up to the pharmacist. They might swap it. They might not. It depends on their judgment, the pharmacy’s policy, or whether they think you’ll say yes. This isn’t just about cost. It’s about behavior. A 2011 study tracked simvastatin prescriptions after the brand patent expired. In mandatory states, 48.7% of prescriptions were filled with the generic. In permissive states? Only 30%. That’s nearly a 20-point gap. And when states required patient consent before substitution, generic use dropped even further-to just 32.1%.Why Do Some States Make It Harder to Swap?
It’s not random. States with stricter rules often have extra layers: patient consent, mandatory notifications, or liability fears. Thirty-one states and Washington, D.C. require pharmacists to tell you in writing-separate from the drug label-that a substitution happened. That means a note on the receipt, a sticker on the bottle, or even a verbal warning. It sounds helpful, but it adds steps. Pharmacists in those states are less likely to swap at all, especially for drugs with narrow therapeutic indexes-medications like warfarin or thyroid pills where even small changes can cause big problems. Seven states plus D.C. go further: they require your explicit consent before swapping. You have to say yes. Out loud. Or in writing. In those places, pharmacists are nearly twice as likely to skip substitution entirely, even when it’s safe. Why? Because they’re afraid of being blamed if something goes wrong. And in 24 states, there’s no legal shield protecting them from liability if a patient has a bad reaction after a generic is given. That’s a big reason why pharmacists play it safe.How Do Prescribers Control the Swap?
Doctors have the final say-but how they say it varies wildly. In some states, if a doctor writes “Dispense as Written” or “Do Not Substitute” on the prescription, that’s it. No swap. In others, like California or Texas, the default is substitution unless the doctor writes “Brand Medically Necessary.” That’s a subtle but powerful difference. One puts the burden on the doctor to stop the swap. The other puts the burden on the doctor to allow it. Some states even require two-line prescriptions: one line for the drug name, another for the prescriber’s signature that says “Substitution Permitted.” If the doctor doesn’t sign the second line, the pharmacist can’t swap. Other states don’t have that format at all. So if you’re a doctor in one state and your patient moves to another, the same prescription might be treated completely differently.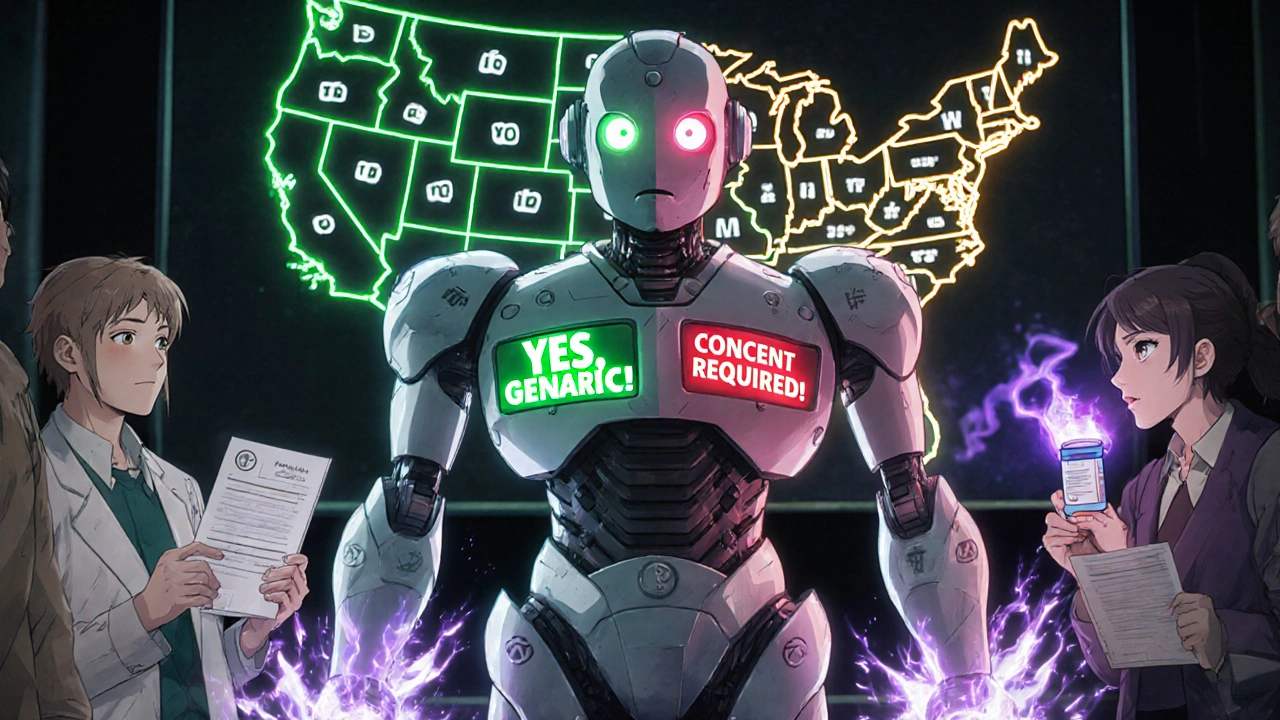
Biosimilars Are a Whole Different Game
Generic drugs are copies of small-molecule pills-like atorvastatin or metformin. Biosimilars are copies of complex biologic drugs-like Humira or Enbrel. These aren’t simple copies. They’re made from living cells. Even tiny differences can trigger immune reactions. Because of that, 45 states treat biosimilars much more carefully than regular generics. Most require the doctor to specifically approve each switch. Some require the pharmacy to notify the doctor before swapping. A few even demand that the patient be tracked over time after the switch. Only nine states and D.C. apply the same rules to biosimilars as they do to regular generics. That’s because the stakes are higher. Biologics cost tens of thousands of dollars a year. But they’re also riskier to swap. So states are erring on the side of caution-even if it slows down cost savings.What This Means for You
If you’re on a generic medication and you move states, your refill might get blocked-or you might suddenly get switched without warning. In mandatory states, you’ll likely get the generic every time. That’s good for your wallet. But if you’re on a narrow therapeutic index drug, you might want to ask your doctor to write “Dispense as Written” just to be safe. In permissive states, you might get the brand every time unless you ask for the generic. Don’t assume the pharmacist will offer it. Ask. Say: “Is there a generic version? Can I get it?” If you’re on a biologic, check your state’s rules. Some states require your doctor to sign off every time. Others let the pharmacist decide. Know what you’re entitled to.
Why This Matters for Healthcare Costs
Generic drugs cost 80-85% less than brand-name versions. That’s not a small savings. In 2011, the Congressional Budget Office estimated that increasing generic use by just 1% would save Medicare Part D $160 million a year. States with mandatory substitution save more. Medicaid programs in those states see higher generic use, fewer refills, and lower overall spending. But those savings come with trade-offs. More substitutions mean more pharmacist workload. More paperwork. More potential for errors. The system isn’t perfect. But the data shows one clear thing: when substitution is automatic, people take their meds more often. When it’s optional, people skip doses, forget, or just don’t fill the prescription because it’s too expensive.What’s Changing?
Since 2014, the number of mandatory substitution states has gone from 14 to 19. That’s a trend. More states are realizing that letting pharmacists swap generics isn’t risky-it’s responsible. It’s cheaper. It’s better for public health. But as new drugs like biosimilars and combination therapies enter the market, states are adding new rules. Some are creating “positive formularies” that list which drugs can be swapped. Others are banning substitutions for certain high-risk drugs altogether. The bottom line? The rules are still messy. But they’re moving in one direction: toward more substitution, not less.Can a pharmacist refuse to substitute a generic drug even in a mandatory state?
Yes, but only under specific exceptions. Even in mandatory substitution states, pharmacists can refuse to swap if the prescriber has written “Dispense as Written” or “Brand Medically Necessary” on the prescription. They can also refuse if the brand-name drug is priced the same as the generic, if the patient refuses, or in emergency situations where the generic isn’t immediately available. Some states also exempt narrow therapeutic index drugs unless the prescriber approves the switch.
Do I have to pay more if I get the brand-name drug instead of the generic?
Often, yes. Most insurance plans require you to pay the full difference between the brand and generic price if you choose the brand. For example, if the generic costs $10 and the brand costs $120, your copay might jump from $10 to $110. Some plans even refuse to cover the brand at all unless your doctor proves it’s medically necessary. Always check your plan’s formulary before assuming you’ll get the brand for free.
Why do some states require patient consent for substitution?
These rules were originally created out of concern for patient safety, especially with drugs that have narrow therapeutic indexes. The idea was that patients should be informed and agree before a change is made. But studies show these consent requirements backfire: they reduce generic use dramatically without improving safety. Patients often don’t understand the difference between brand and generic, so they say no out of confusion or fear. In practice, these rules protect brand manufacturers more than patients.
How do I find out what my state’s substitution laws are?
Your state’s Board of Pharmacy website is the most reliable source. Most have a section on pharmacy laws or generic substitution. You can also ask your pharmacist directly-they’re required to know the rules. For a quick overview, search “[Your State] generic substitution law 2025.” The National Association of Boards of Pharmacy also publishes annual summaries that track these laws across all states.
Can I ask for a generic even if my state is permissive?
Absolutely. You have the right to request a generic drug at any time, regardless of state law. Just tell the pharmacist: “I’d like the generic version if it’s available and approved.” Many pharmacists will offer it anyway, especially if it saves you money. If they say no, ask why. If it’s because they don’t have it in stock, they can order it. If they say it’s not allowed, they’re mistaken-permissive means they can, not that they must refuse.


Lisa Detanna
November 23, 2025 AT 09:48So let me get this straight - in some states, you need to beg for a generic drug like it’s a favor? That’s insane. I’ve had pharmacists act like they’re doing me a personal favor by giving me the cheaper version. Meanwhile, my wallet’s crying and my doctor’s just shrugging. This isn’t healthcare - it’s a lottery.
And don’t even get me started on biosimilars. If we’re talking about life-saving meds that cost $10K a year, why are we treating them like fragile glass figurines? We’re not swapping out cereal brands here. We’re talking about people skipping doses because they can’t afford the brand. That’s not caution - that’s cruelty dressed up as policy.
Demi-Louise Brown
November 23, 2025 AT 22:11Generic substitution policies vary significantly across jurisdictions and reflect differing interpretations of patient safety, cost efficiency, and professional autonomy. The data cited indicates a clear correlation between mandatory substitution and increased generic utilization. However, the absence of standardized protocols for communication and documentation may introduce unintended barriers to adherence.
Matthew Mahar
November 24, 2025 AT 04:48ok so i just got my thyroid med switched and i had no idea it happened until i checked the bottle and it was a different color?? like bro i dont even know what a generic is but i know my pills dont look like that anymore and now im paranoid i’m gonna have a heart attack??
why is this so complicated?? why do i need a PhD just to fill a prescription??
John Mackaill
November 25, 2025 AT 04:37The disparity in substitution laws reflects a deeper tension between public health goals and liability aversion. States requiring consent may intend to empower patients, but in practice, they often reinforce misinformation and reduce access. The real issue isn’t patient autonomy - it’s the lack of clear, accessible education about bioequivalence.
Pharmacists are gatekeepers, not decision-makers. The system needs to equip them with tools, not handcuffs.
Adrian Rios
November 26, 2025 AT 13:12Look, I get why some states are scared - biologics are complex, and if someone has a bad reaction, the pharmacy could get sued into oblivion. But here’s the thing: the FDA approves generics and biosimilars after years of testing. They’re not ‘kinda close’ - they’re proven. So why are we letting fear dictate access?
And don’t tell me it’s about safety. If that were true, we’d ban all new drugs until we had 20 years of data. We don’t. We let doctors prescribe them. So why can’t pharmacists dispense them?
The real problem? Insurance companies and pharma lobbyists. They don’t want generics to be easy. Because if you can just grab the cheaper version without jumping through ten hoops, their profits shrink. And guess who pays? The patient. The elderly. The diabetic. The asthmatic kid whose mom can’t afford the brand. This isn’t about science. It’s about money. And it’s broken.
Also - if your doctor wrote ‘Dispense as Written’ on a script in Texas, but you move to Alabama, your script gets auto-swapped anyway. So now you’ve got two systems that don’t talk to each other. How is that not a disaster waiting to happen?
And why is there no national database? Why do I need to Google ‘[my state] generic substitution law 2025’ like I’m doing homework? This is healthcare. It should be seamless. It should be simple. It’s not. And that’s unacceptable.
Casper van Hoof
November 27, 2025 AT 01:03The structural asymmetry between mandatory and permissive substitution regimes reveals a normative assumption: that patient agency is best preserved through procedural complexity. Yet empirical evidence suggests that such complexity diminishes actual agency by introducing cognitive overload, informational asymmetry, and institutional inertia. The paradox lies in the fact that policies designed to protect autonomy frequently result in its erosion.
Richard Wöhrl
November 28, 2025 AT 22:11Important note: In states with mandatory substitution, pharmacists are still required to notify patients - even if they can’t refuse the swap. That notification isn’t optional. And in many cases, they’re required to document it in writing, even if it’s just a sticker on the bottle.
Also - if you’re on a narrow therapeutic index drug (like warfarin, levothyroxine, or phenytoin), you should ALWAYS ask your doctor to write ‘Dispense as Written’ - even in mandatory states. Why? Because some pharmacists still hesitate, and some insurance systems don’t flag those drugs properly.
And yes - if you’re on a biosimilar, you’re probably in a state that requires extra steps. Check your state’s board of pharmacy website. Don’t assume. Ask. Write it down. Keep a copy in your phone. This stuff matters.
Also - if your pharmacist says ‘We can’t substitute this,’ ask them why. If they say ‘It’s not allowed,’ they’re probably wrong. Permissive doesn’t mean ‘no,’ it means ‘maybe.’ And you have the right to say ‘yes.’
Pramod Kumar
November 29, 2025 AT 13:27Bro, this whole system feels like someone took a blender, threw in a pharmacy, a law book, and a Walmart receipt, and hit puree.
In India, we don’t even have brand names - everything’s generic. You get the same pill, same effect, same price. No drama. No stickers. No consent forms.
Here, we’re making people jump through hoops to save money. That’s backwards. We’re punishing the poor for being poor. And we call it ‘care.’
Also - why does the pharmacist know more about my meds than my doctor? That’s not right. Someone needs to fix this.
Brandy Walley
November 30, 2025 AT 03:36Wow. So now we’re letting pharmacists play doctor? Next they’ll be writing prescriptions. This is why America is falling apart. People think generics are ‘the same’ - they’re not. They’re knockoffs. Like fake designer bags. You think you’re saving money but you’re just getting junk.
My cousin took a generic and got sick. Now she’s on disability. You think that’s worth $10?
shreyas yashas
December 1, 2025 AT 22:03Simple truth: if you don’t ask, you don’t get. I’m from India, moved here 3 years ago. First time I asked for generic, pharmacist looked at me like I asked for a unicorn.
Now I say it loud: ‘Generic? Please.’
9 times out of 10, they say yes.
Stop waiting for the system to fix itself. You’re the customer. Ask.
Suresh Ramaiyan
December 2, 2025 AT 08:48There’s a quiet irony here: we demand transparency in our food, our cars, our phones - yet when it comes to the medicine that keeps us alive, we treat it like a secret ritual. The pharmacist holds the key, but the patient is never told the code.
What if we treated drug substitution like software updates? You get a notification: ‘Your medication has been updated to a newer, cheaper version. Same active ingredient. FDA-approved. 85% cheaper. Would you like to proceed?’
No forms. No fear. Just clarity.
Why can’t healthcare be this simple?
Katy Bell
December 2, 2025 AT 09:28Just had this happen to me last week. Got my blood pressure med - same pill, different color, different shape. I didn’t say anything. I just took it. But I felt weird. Like I was taking someone else’s medicine.
Then I read this post.
Turns out I’m in a mandatory state. So they HAD to switch me.
But nobody told me. Not the pharmacist. Not the doctor. Not the insurance.
I’m fine. No side effects.
But I’m mad.
Why don’t they just say something?
It’s not about the pill.
It’s about being treated like a person.