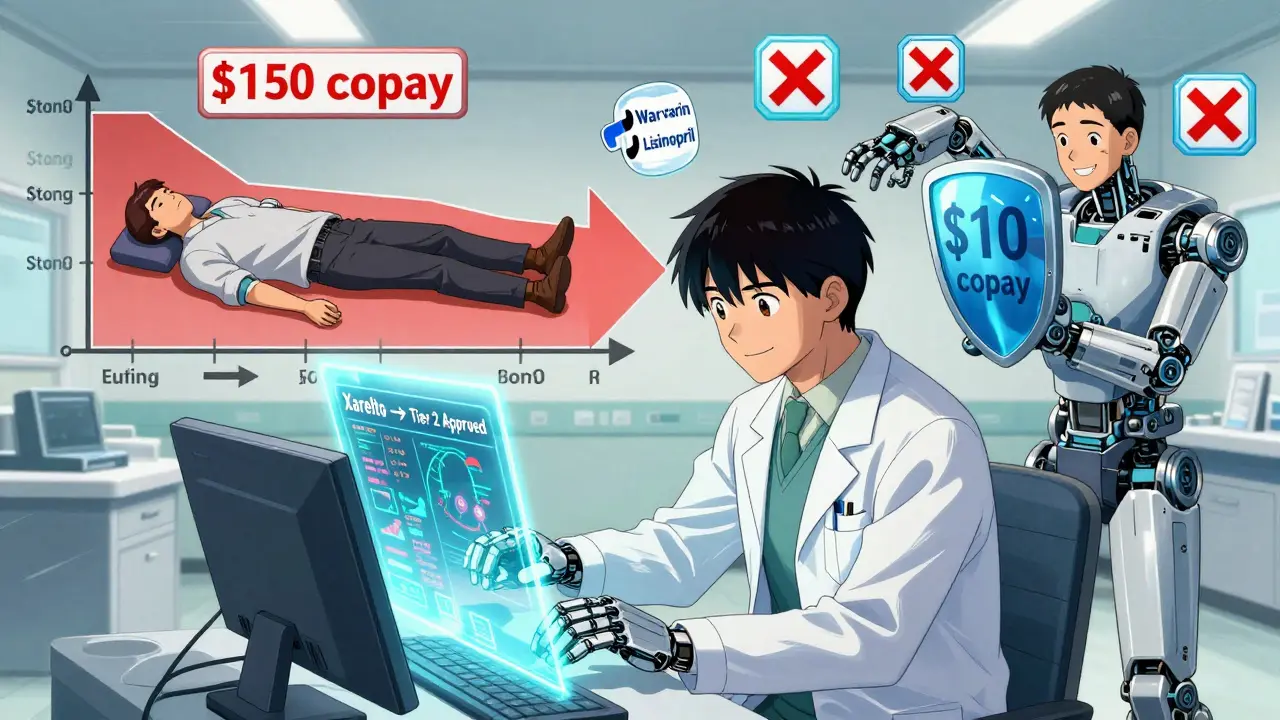
When you pick up your prescription and see the copay is $150 instead of the $20 you expected, it’s not a mistake - it’s likely because your drug is on a higher tier. Many Medicare Part D plans use a tiered system to control costs, putting medications into different price levels. But here’s the thing: tier exceptions can cut those costs dramatically - sometimes to zero. And most people don’t even know they exist.
What Exactly Is a Tier Exception?
A tier exception is a formal request to your Medicare drug plan to move a medication from a higher-cost tier to a lower one. It’s not about getting a drug that’s not on the formulary. It’s about getting the drug you’re already prescribed - but at a cheaper price. For example, if your drug is on Tier 4 (where you pay $100 or more per month), a successful tier exception could move it to Tier 1, where you pay $0 or $10. That’s not a small difference. It’s $1,200 a year saved on one prescription. According to the Medicare Rights Center, beneficiaries who successfully use tier exceptions save an average of $37.50 per fill. For someone on multiple medications, that adds up fast. The system was created in 2006 under Medicare Part D. The idea was simple: encourage patients to use lower-cost drugs by making them cheaper. But it didn’t account for everyone’s medical needs. That’s where tier exceptions come in. They’re the safety valve - letting patients get the right drug, not just the cheapest one.How Drug Tiers Work (And Why You’re Paying More)
Most Medicare Part D plans have 4 or 5 tiers. Here’s what they usually look like:- Tier 1: Generic drugs - $0 to $15 copay
- Tier 2: Preferred brand-name drugs - $10 to $40 copay
- Tier 3: Non-preferred brand-name drugs - $50 to $100 copay
- Tier 4: Preferred specialty drugs - 20% to 30% coinsurance (often $100-$300/month)
- Tier 5: Non-preferred specialty drugs - 30% to 40% coinsurance ($500-$1,500/month)
When a Tier Exception Makes Sense
You should consider a tier exception if:- You’re on a drug that’s not working well on a lower-tier alternative
- You had a bad reaction to a preferred drug - like severe nausea, rash, or dizziness
- Your current drug is the only one that controls your condition
- You’re taking a specialty drug (like for MS, cancer, or autoimmune diseases)
- You’re approaching the coverage gap (donut hole) and want to avoid higher coinsurance
- A patient on Xarelto for blood clots was paying $45/month on Tier 3. After a tier exception, they got moved to Tier 2 - paying $10/month.
- Another patient on Copaxone for multiple sclerosis dropped from $1,200/month (Tier 5) to $60/month (Tier 2) after submitting clinical notes showing previous drugs caused severe liver damage.
How to Request a Tier Exception - Step by Step
This isn’t something you do alone. You need your doctor on your side. Here’s how it works:- Check your copay. If it’s higher than expected, ask your pharmacist if your drug is on a high tier. They can tell you which tier it’s on.
- Talk to your doctor. Say: “I can’t afford this copay. Can we file a tier exception to move this drug to a lower tier?”
- Your doctor fills out the form. Most plans have a standard form. Some allow electronic submission through their portal. The form asks why the preferred drugs won’t work for you.
- Your doctor writes a clinical justification. This is the key. Don’t let them write vague stuff like “patient prefers this drug.” That gets denied. They need to say:
- “Patient developed gastrointestinal bleeding on Warfarin, requiring hospitalization.”
- “Patient has severe allergic reaction to all sulfa-based drugs, making this the only viable option.”
- “Previous attempts with Tier 1 and Tier 2 alternatives failed to control symptoms, resulting in two ER visits.”
Specificity wins. Evidence wins. Documentation wins.
- Submit the request. Your doctor’s office usually submits it. Some plans let you submit it online. Either way, make sure you get a confirmation number.
- Wait for a decision. Standard requests take up to 14 days. If your health is at risk (like if you’re about to stop a critical medication), ask for an expedited review - they must respond in 72 hours.
- If denied, appeal. Don’t give up. The Medicare Rights Center says 78% of denied requests are approved on appeal - if you add more clinical evidence.
What Gets Approved - And What Doesn’t
Approved exceptions almost always involve:- Chronic conditions: rheumatoid arthritis, lupus, MS, heart failure
- Drugs with serious side effects on alternatives
- Patients who’ve tried and failed lower-tier options
- Medications with unique dosing or delivery methods (like injectables or infusions)
- Specific clinical language
- Proof that alternatives failed
- Documentation of adverse reactions
- Doctor’s signature or contact info
Timing Matters - Do This Before You Fill the Script
Waiting until you’ve paid $150 for your first fill is a mistake. The best time to request a tier exception is before you fill the prescription. Why? Because:- If approved, you pay the lower copay from day one
- If denied, you still have time to ask your doctor for an alternative
- You avoid paying out-of-pocket money that you might not get back
What to Do If You’re Denied
Denials happen - even with good documentation. But you’re not out of options.- Request a redetermination. This is your first appeal. You have 60 days from the denial date.
- Add more evidence. Send lab results, hospital records, or specialist letters. Don’t just say “my doctor says so.” Show proof.
- Ask for a peer-to-peer review. Some plans let your doctor speak directly to the insurer’s medical director. This works - especially for complex cases.
- Call your State Health Insurance Assistance Program (SHIP). They offer free counseling. Find yours at shiptacenter.org.
What’s Changing in 2025 and Beyond
Starting in 2025, the Inflation Reduction Act will cap out-of-pocket drug costs at $2,000 per year for Medicare beneficiaries. That’s huge. But it doesn’t mean tier exceptions disappear. Why? Because:- The $2,000 cap kicks in after you’ve spent that much - so lowering your monthly copay still helps you get there faster
- Some plans still charge coinsurance (not copays) on specialty drugs - tier exceptions can turn 40% coinsurance into a flat $10 copay
- Non-Medicare plans (like employer coverage) still use tiering - and tier exceptions work the same way
Final Tips to Maximize Your Savings
- Always ask your pharmacist: “What tier is this drug on?”
- Keep a copy of every form and denial letter - you’ll need them if you appeal
- Don’t wait until you’re in the donut hole - act early
- If your doctor says “I don’t do exceptions,” find another doctor - or ask them to refer you to someone who does
- Use free help: Call 1-800-MEDICARE or visit your local SHIP office
Tier exceptions aren’t a loophole. They’re a rule built into the system - designed to protect people who need specific drugs. If you’re paying more than you should for a medication that works for you, you’re not alone. But you’re also not powerless.
What’s the difference between a tier exception and a formulary exception?
A tier exception is for a drug that’s already on your plan’s formulary but is on a higher, more expensive tier. You’re asking to move it to a lower tier. A formulary exception is for a drug that’s not on the formulary at all - you’re asking to get it covered at all. Tier exceptions are easier to get because the drug is already approved; you just need a lower price.
Can I request a tier exception for any medication?
Yes - as long as the drug is on your plan’s formulary. You can’t request a tier exception for a drug that’s completely excluded. But if it’s listed, even on Tier 5, you can ask to move it to Tier 1, 2, or 3. Most requests are for brand-name and specialty drugs that cost over $50 per month.
Does my doctor have to submit the request?
Yes. Only your prescribing doctor (or their authorized representative) can provide the clinical justification needed. You can submit the form, but without your doctor’s signature and medical reasoning, the request will be denied. Don’t try to do it yourself - your doctor’s input is what makes it work.
How long does a tier exception take to process?
Standard requests take up to 14 days. If your doctor says your health is at risk - like if you’re about to stop a life-sustaining drug - you can request an expedited review. In that case, the plan must respond within 72 hours. Always ask for expedited if you’re in a time-sensitive situation.
What if I’ve already paid for my medication?
If you paid out-of-pocket and then get approved, you can ask for a refund. Submit a copy of your receipt and the approval letter to your plan. Most plans will refund the difference between what you paid and what you should have paid under the lower tier. It’s not automatic - you have to ask.
Can I get a tier exception for a drug I’ve been taking for years?
Yes. Even if you’ve been on the same drug for 10 years, if your plan changed its formulary or moved your drug to a higher tier, you can still request an exception. Insurance plans update their formularies every year. Your drug might have been on Tier 1 last year and moved to Tier 3 this year. That’s when you act.

