Medication Side Effect Tracker
How to Use This Tool
Enter your medication start date and symptom onset date to see if they match patterns for common side effects. Remember: Never stop medications without consulting your doctor.
Timing Analysis Results
Enter dates to see analysis...
It’s one of the most confusing and scary things you can experience: you start a new medication, and suddenly you feel worse. Is your condition getting worse? Or is it the medicine? This isn’t just a minor worry - it’s a real clinical problem. About 40% of people with chronic illnesses misattribute their medication side effects as signs their disease is progressing. That leads to unnecessary tests, extra pills, and sometimes serious harm.
The difference between a disease symptom and a medication side effect sounds simple, but in practice, it’s not. Both can make you tired, dizzy, nauseous, or anxious. The key isn’t just what you feel - it’s when you feel it, how it changes, and what else is going on in your body.
What Exactly Is a Side Effect?
A side effect is an unintended reaction to a drug that happens at normal doses. It’s not an overdose. It’s not a mistake. It’s a known, predictable response built into how the drug works in your body. The World Health Organization defines it clearly: any unintended response to a medication taken for treatment, prevention, or diagnosis.
Some side effects are mild and temporary - like dry mouth from an antihistamine or nausea when starting an antidepressant. Others can be more serious - weight gain from antipsychotics, persistent cough from blood pressure meds like lisinopril, or sexual dysfunction from SSRIs like sertraline. The good news? Most mild side effects fade after a few weeks as your body adjusts. The bad news? Many people don’t know that, so they stop taking their meds too soon.
What Counts as a Disease Symptom?
Disease symptoms are the direct result of your underlying condition. If you have depression, fatigue, low motivation, trouble sleeping, and trouble concentrating are core symptoms - not side effects. If you have high blood pressure, headaches or dizziness might be signs your pressure is dangerously high. If you have arthritis, joint swelling and stiffness are the disease itself.
These symptoms follow the natural course of the illness. They don’t suddenly appear the day after you start a new pill. They build slowly over time, or they flare up due to triggers like stress, infection, or lack of sleep. They don’t disappear when you lower your dose - unless the medication is actually treating the condition.
Timing Is Everything
This is the single most useful clue. Side effects almost always show up after you start a new drug - usually within days to four weeks. If you’ve been on a medication for six months and suddenly feel new symptoms, it’s less likely to be the drug.
Here’s how timing breaks down:
- Immediate (minutes to hours): Drowsiness from allergy meds, dizziness from blood pressure pills, flushing from niacin.
- Delayed (days to weeks): Weight gain from antidepressants, dry cough from ACE inhibitors, insomnia from SSRIs.
- Chronic (months to years): Bone thinning from long-term steroids, kidney changes from NSAIDs.
If your new symptom matches one of these patterns - especially if it started right after you began the medication - it’s a strong signal it’s a side effect.
Dose Matters
Side effects usually get worse when you increase the dose - and better when you lower it. That’s called a dose-response relationship. If your headache gets worse every time your doctor bumps up your antidepressant, that’s a red flag.
Disease symptoms don’t follow this pattern. Your arthritis pain won’t suddenly spike because you took an extra 5mg of your blood pressure pill. But if you start feeling worse when you take more of a drug - and better when you take less - that’s textbook side effect behavior.
Drug Classes Have Signature Side Effects
Not all drugs cause the same problems. Certain classes have well-known, predictable side effects:
- SSRIs (sertraline, fluoxetine): Sexual dysfunction (30-70% of users), nausea, insomnia, agitation.
- ACE inhibitors (lisinopril, enalapril): Dry cough (5-20%), high potassium, dizziness.
- Antipsychotics (olanzapine, risperidone): Weight gain (4-6 kg in first 12 weeks), drowsiness, metabolic changes.
- Statins (atorvastatin, simvastatin): Muscle aches, liver enzyme changes, rare but serious muscle damage.
- Anticholinergics (diphenhydramine, oxybutynin): Confusion, memory problems, dry mouth - especially dangerous in older adults.
If you’re on one of these drugs and you’re experiencing one of these common reactions, it’s not random. It’s expected. That doesn’t mean it’s harmless - but it does mean it’s likely not your disease acting up.
What About Allergic Reactions?
These are different from side effects. Allergies are immune system reactions. They’re not dose-dependent. They can happen the first time you take a drug - or the tenth. Signs include:
- Hives or rash
- Itchy skin or swelling (especially lips, tongue, face)
- Wheezing or trouble breathing
- Drop in blood pressure
If you have any of these, stop the drug and get help immediately. This isn’t a side effect - it’s an emergency.
How to Tell the Difference: A Simple 4-Step Method
Doctors use structured tools to sort this out. You can use a simpler version at home - but always talk to your provider before making changes.
- Track timing. Write down when you started the drug and when the symptom began. If they line up within 1-4 weeks, side effect is likely.
- Check your dose. Did you recently increase your dose? Did the symptom get worse? That’s a side effect clue.
- Look for patterns. Does the symptom match known side effects for your drug? Use your pharmacy’s patient guide or trusted sites like MedShadow.org.
- Test it out (with your doctor). The most reliable way? A temporary stop - called a “dechallenge.” If the symptom fades after stopping the drug, and comes back when you restart it (a “rechallenge”), that’s strong proof it’s a side effect. This must be done under medical supervision.
Why People Get It Wrong
There’s a reason this confusion is so common. Many symptoms overlap. Fatigue? Could be depression. Could be an SSRI. Headaches? Could be high blood pressure. Could be a beta-blocker. Insomnia? Could be anxiety. Could be an antidepressant.
Studies show that 32% of patients with chronic conditions think their worsening symptoms mean their disease is getting worse - when it’s actually the medicine. In older adults, this is especially dangerous. About 15-20% of new dementia diagnoses in seniors turn out to be side effects from medications like antihistamines or bladder pills - not Alzheimer’s.
And let’s not forget polypharmacy. If you’re taking five or more drugs - which 35% of adults over 65 do - the chances of drug interactions causing confusing symptoms go way up. One pill might cause drowsiness. Another might cause forgetfulness. Together? It looks like dementia.
What You Can Do Right Now
You don’t need to be a doctor to spot the difference. Here’s what works:
- Keep a symptom journal. Write down: what you took, when, how much, and what you felt - along with severity (1-10 scale). Do this for at least two weeks. You’ll start seeing patterns.
- Use a medication app. Apps like Medisafe let you log pills and symptoms side by side. Studies show people who use them identify side effects 34% faster.
- Ask your pharmacist. They know the side effect profiles of every drug you take. Bring your list to them - even if you’re not sure what’s wrong.
- Don’t stop cold turkey. Stopping antidepressants, blood pressure meds, or seizure drugs suddenly can be dangerous. Always talk to your doctor first.
- Ask: “Could this be the medicine?” Don’t assume it’s your disease. Push for a side effect review. You’re not being difficult - you’re being smart.
Technology Is Helping
Hospitals now use tools that flag possible side effects based on your age, other meds, and health history. Epic’s Drug Interaction Module, used by 67% of U.S. hospitals, spots risks with 82% accuracy. The FDA’s Sentinel system tracks millions of patient records to catch side effects that doctors miss.
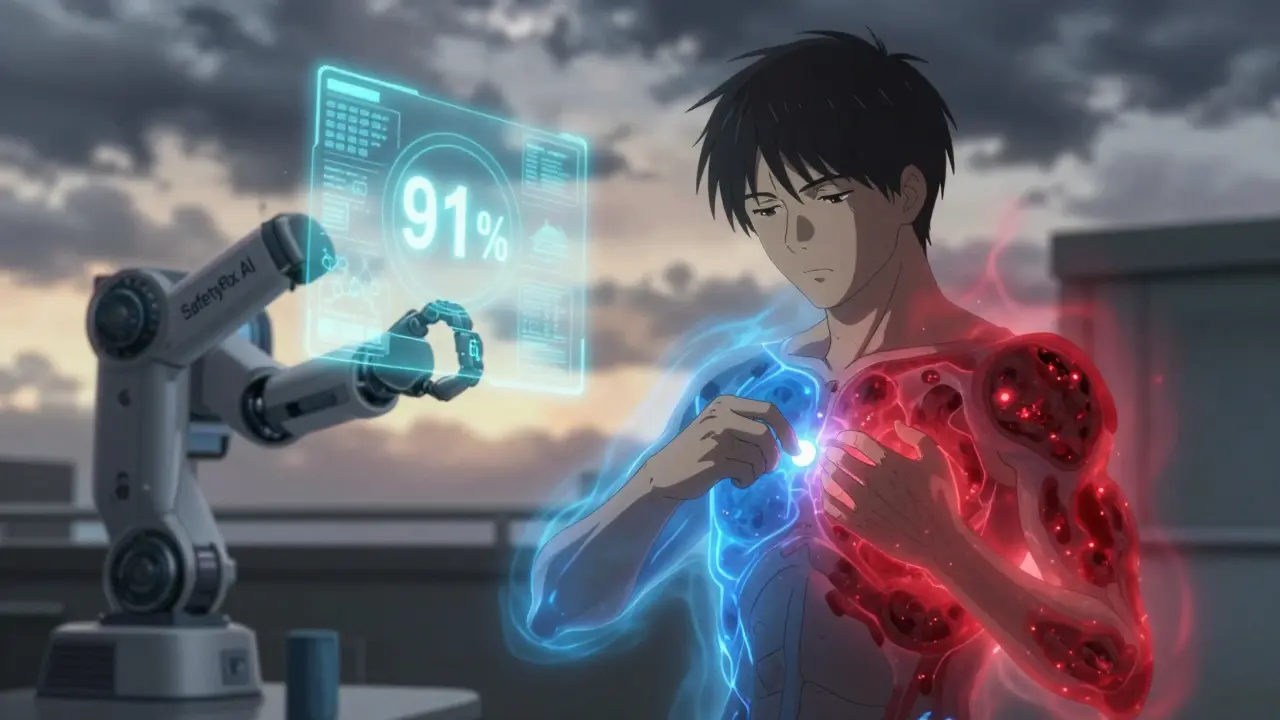
Even AI is stepping in. MedAware’s SafetyRx tool, approved by the FDA in 2022, analyzes your electronic records and predicts whether a symptom is likely a side effect or disease flare - with 91% accuracy. And pharmacogenomic testing - which checks your genes to see how you’ll react to certain drugs - is now covered by most insurers for high-risk meds. It can cut misattribution by nearly half.
Bottom Line
You’re not imagining things. If you feel worse after starting a new medication, it might not be your disease - it might be the treatment. The good news? Most side effects are manageable. Many fade. Some can be fixed by lowering the dose or switching drugs.
But you won’t know unless you track, question, and talk. Don’t let fear keep you silent. Don’t assume your doctor will catch it. Keep a journal. Note the timing. Compare it to known side effects. Ask the question: “Could this be the pill?”
That one question could save you from unnecessary tests, extra meds, and months of unnecessary suffering.
How do I know if my nausea is from my medication or my illness?
Nausea is one of the most common side effects - it happens in 25-30% of people starting new meds. If the nausea started within a few days of beginning the drug, it’s likely the medication. If you’ve had nausea for months before starting the drug, it’s probably your illness. Keep a log: write down when you took the pill and when you felt sick. If the nausea improves after a week or two, it’s probably your body adjusting. If it keeps getting worse or doesn’t go away, talk to your doctor - you may need a different drug or a lower dose.
Can side effects show up months after starting a drug?
Yes. While most side effects appear within the first few weeks, some take months or even years. Weight gain from antipsychotics, bone loss from long-term steroids, and kidney changes from NSAIDs can develop slowly. If you notice a new, unexplained change after months on a drug - especially if it’s something not typical for your condition - it’s worth discussing. Don’t assume it’s just aging or your disease progressing.
Why do some side effects go away over time?
Your body adapts. Many side effects - like drowsiness from antihistamines, nausea from SSRIs, or dizziness from blood pressure meds - happen because your system isn’t used to the drug. Over time, your liver processes it differently, your brain adjusts its receptors, and your body finds a new balance. That’s why 60-70% of mild side effects fade on their own within a few weeks. But if it’s a side effect that doesn’t fade - like sexual dysfunction or persistent cough - it won’t go away unless you change the drug.
Is it safe to stop a medication if I think it’s causing side effects?
No - not without talking to your doctor first. Stopping antidepressants, blood pressure pills, seizure meds, or steroids suddenly can cause dangerous withdrawal symptoms or make your original condition worse. Instead, keep a symptom log and schedule a visit. Your doctor can help you safely reduce the dose, switch drugs, or confirm whether it’s really the medication. Never quit cold turkey.
Can two medications cause the same side effect?
Absolutely. If you’re taking more than one drug, side effects can add up. For example, both an SSRI and a sleep aid can cause drowsiness. Two different blood pressure pills might both lower your blood pressure too much, making you dizzy. This is called cumulative side effects. If you’re on five or more meds, you’re at higher risk. Always review your full list with your pharmacist - they can spot hidden interactions you might miss.
What should I bring to my doctor to help them figure this out?
Bring your complete medication list - including supplements and over-the-counter drugs - along with your symptom journal. Note: when each symptom started, how often it happens, how bad it is (1-10), and whether it changed after a dose adjustment. If you use a health app, show them the data. The more specific you are, the faster they can tell if it’s your disease or your meds.


Wendy Claughton
January 18, 2026 AT 10:40Stacey Marsengill
January 19, 2026 AT 06:03Robert Davis
January 20, 2026 AT 06:41Eric Gebeke
January 21, 2026 AT 08:55Jake Moore
January 21, 2026 AT 19:20Praseetha Pn
January 22, 2026 AT 12:50Nishant Sonuley
January 22, 2026 AT 13:12Emma #########
January 23, 2026 AT 01:38Andrew McLarren
January 25, 2026 AT 00:04Andrew Short
January 25, 2026 AT 13:37christian Espinola
January 26, 2026 AT 23:06