Every pill, syrup, or patch you take comes with a label. But how many of us actually read it properly? You might grab your medicine, swallow it, and move on - but skipping the fine print could mean taking too much, too little, or mixing dangerous combinations. Medication errors are one of the leading causes of preventable harm in homes and hospitals. In the U.S. alone, about 1.5 million people suffer preventable adverse drug events each year because they misunderstood their label. And it’s not just about pills - liquid meds, patches, and even OTC pain relievers can be risky if you don’t know what you’re looking at.
What’s on a Medication Label?
Medication labels aren’t random text. They follow strict rules set by the FDA. Whether it’s a prescription from your doctor or a bottle from the pharmacy shelf, the label has specific sections you need to know.For prescription drugs, the label includes 16 required sections. The most important one for you is Dosage and Administration. This tells you exactly how much to take, how often, and under what conditions. For example, it might say: "Take 1 tablet by mouth every 12 hours" - or it might warn you: "Do not take if creatinine clearance is below 30 mL/min". That second part sounds complicated, but it’s there to protect you if your kidneys aren’t working normally.
For over-the-counter (OTC) medicines like Tylenol or Advil, labels follow the Drug Facts format. This is simpler and easier to scan. You’ll see seven key parts:
- Active Ingredient: The actual medicine in the bottle (e.g., acetaminophen 500mg).
- Purpose: What it does (pain reliever, antihistamine, etc.).
- Uses: What it treats (headache, fever, runny nose).
- Warnings: Red flags - what to avoid, who shouldn’t take it, and possible side effects.
- Dosage: How much and how often to take it.
- Other Information: Storage tips, expiration date, inactive ingredients.
- Inactive Ingredients: Fillers, dyes, flavors - important if you have allergies.
One thing you’ll always find: the expiration date. That’s not just a suggestion. After that date, the medicine may not work as well - or could break down into something harmful. Prescription meds usually expire one year after the pharmacy dispenses them. OTC meds last longer, often 2-3 years from manufacture, but don’t assume they’re safe past the printed date.
Understanding Dosage: More Than Just "Take Two"
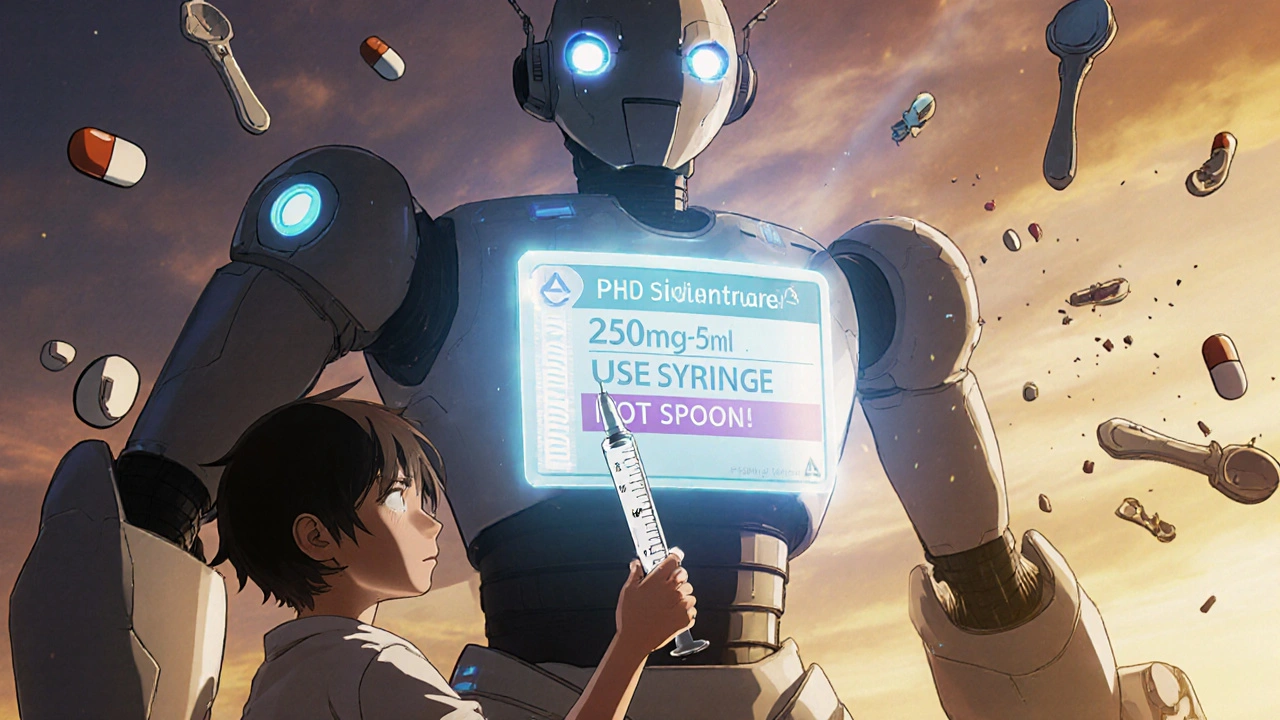
"Take two tablets every 6 hours" sounds simple. But what if you’re taking three different medicines - and two of them have the same active ingredient? That’s how people accidentally overdose on acetaminophen. It’s in Tylenol, cold meds, sleep aids, even some prescription painkillers. You might think you’re being careful by spacing them out - but if you’re taking two different products with acetaminophen, you could hit the 4,000mg daily limit without realizing it.For children, dosage is often based on weight, not age. If your child weighs 15kg, and the label says "5-10mg per kg per dose," you need to calculate: 15 × 5 = 75mg minimum, 15 × 10 = 150mg maximum. If the liquid is 160mg per 5mL, then 75mg is about 2.3mL. That’s why using a dosing syringe - not a kitchen spoon - is critical. Household spoons vary wildly in size. A "teaspoon" can be anywhere from 2.5mL to 7.3mL. That’s a 200% difference. One wrong spoon can mean a dangerous overdose.
With liquid medications, you also need to understand concentration. A label might say: "250mg per 5mL". That means each milliliter has 50mg. If your doctor orders 500mg, you need 10mL - not 5mL. Many parents get this wrong. One pharmacist in Adelaide told me about a mom who gave her toddler the entire 30mL bottle of amoxicillin because she thought "5mL" meant "one dose," not "each 5mL is one dose." That child ended up in the ER.
Why Warnings Matter More Than You Think
The "Warnings" section is where most people skim - and that’s where the biggest risks hide.Take ibuprofen. The warning might say: "Do not use if you have a history of stomach bleeding." Or: "May increase risk of heart attack or stroke." If you’ve had ulcers or high blood pressure, skipping this could be life-threatening.
Another common warning: "Avoid alcohol." That’s not just about getting drunk. Mixing alcohol with certain painkillers, antibiotics, or antidepressants can cause liver damage, dizziness, or even respiratory failure. One study found that 47% of people never read this part.
Some labels warn about drug interactions. For example, if you’re on warfarin (a blood thinner), you can’t take certain cold medicines with pseudoephedrine. Or if you’re on statins, grapefruit juice can turn a safe dose into a toxic one. These aren’t theoretical risks - they happen daily.
The Five Rights of Safe Medication Use
Nurses and pharmacists use a simple system called the Five Rights to prevent errors. You can use it too:- Right Patient: Is the name on the bottle yours? Double-check. Especially if you share meds with family.
- Right Drug: Does the name match what your doctor prescribed? "Amoxicillin" isn’t the same as "Azithromycin."
- Right Dose: Is the amount correct? Don’t guess. Use a measuring tool.
- Right Route: Is it meant to be swallowed, inhaled, or applied to the skin? Putting a pill meant for your mouth under your tongue can change how fast it works.
- Right Time: "Take with food" or "Take on an empty stomach" matters. Some drugs are absorbed better - or safer - when taken with meals.
Every time you take a pill, pause and ask: "Am I checking all five?" It takes 10 seconds. It could save your life.
What to Do When You’re Confused
If the label doesn’t make sense - or if you’re unsure - don’t guess. Don’t rely on memory. Don’t ask a friend.Call your pharmacist. They’re trained to explain labels. Most will walk you through it over the phone. No judgment. No rush. They’ve seen it all: parents confused about kids’ doses, elderly patients mixing 10 different pills, people using old prescriptions because "it worked before."
Some high-risk drugs - like insulin, blood thinners, or cancer meds - come with a Medication Guide. This is a separate printed sheet with plain-language instructions and illustrations. Pharmacists are required to give you this. If they don’t, ask for it. There are over 150 medications that legally require one.
For parents: If your child’s medicine doesn’t come with a dosing syringe, ask for one. Pharmacies give them out free. If you’re using a measuring cup, make sure it has milliliters (mL) - not teaspoons or ounces.

What’s Changing on Labels (And Why It Matters)
The FDA is pushing for simpler, clearer labels. Starting in 2024, more prescriptions will include QR codes that link to videos showing how to use the medicine. In 2021, a pilot program showed that patients who watched these videos made 37% fewer dosing mistakes.By 2027, experts predict all prescription drugs in developed countries will use standardized color-coding. Red = high-risk. Yellow = caution. Green = low-risk. Icons will warn you about drowsiness, sun sensitivity, or alcohol interaction - no reading required.
Right now, labels still vary by brand. One painkiller might say "take every 6 hours," another says "every 4-6 hours." That inconsistency is why so many people get confused. The push for standardization is about safety - not convenience.
Final Checklist: Before You Take Any Medicine
Before you swallow, tap your finger on the bottle and run through this:- Is the name on the bottle my name?
- Is the medicine what my doctor prescribed?
- What’s the active ingredient? Am I taking this elsewhere?
- What’s the exact dose? Do I need a syringe or cup?
- How often? Every 4 hours? Every 12? Always at the same time?
- Any warnings? Food? Alcohol? Other meds?
- Is it expired?
If you can’t answer all of these - don’t take it. Call someone who can help.
What should I do if I accidentally take too much medicine?
If you suspect an overdose, call Poison Control immediately (1-800-222-1222 in the U.S., or your local emergency number). Do not wait for symptoms. Keep the medicine bottle with you when you call - they’ll need the exact name and dose. If the person is unconscious, having seizures, or struggling to breathe, call emergency services right away.
Can I split a pill if the dose is too high?
Only if the pill has a score line (a groove down the middle) and your doctor or pharmacist says it’s safe. Some pills are designed to release medicine slowly - splitting them can cause a dangerous spike in dosage. Never split capsules, extended-release tablets, or coated pills unless explicitly told to. When in doubt, ask for a different strength.
Why do some labels say "take with food" and others say "on an empty stomach"?
Some medicines are absorbed better when food is in your stomach - like antibiotics such as amoxicillin. Others, like thyroid meds or certain antidepressants, can be blocked by food or calcium. Taking them on an empty stomach means no food for 30-60 minutes before and after. Follow the label exactly. Even a small snack can change how well the drug works.
Is it okay to use an old prescription if I still have symptoms?
No. Medications are prescribed for a specific condition, at a specific dose, for a specific time. What worked last time might not be right now - your body, weight, or other meds may have changed. Also, the drug may have expired. Taking old prescriptions can lead to under-treatment, side effects, or antibiotic resistance. Always see your doctor before reusing a prescription.
How do I safely dispose of unused medicine?
Don’t flush pills or throw them in the trash. Many communities have drug take-back programs - check with your local pharmacy or police station. If none are available, mix pills with coffee grounds or cat litter in a sealed bag before throwing them away. This makes them unappealing and unusable. Remove personal info from the bottle before recycling it.
Next Steps: Make Label Reading a Habit
Medication safety isn’t about being perfect. It’s about being aware. Every time you pick up a new prescription or OTC bottle, treat it like a safety manual - because it is. Keep a written list of all your meds, including doses and times. Show it to your doctor and pharmacist at every visit. Ask questions. Write down answers. Don’t be shy.One bottle, one label, one moment of attention - could be the difference between healing and harm. You don’t need to be a doctor to read it. You just need to care enough to try.


Miruna Alexandru
November 23, 2025 AT 02:32The FDA’s Drug Facts format is a marvel of regulatory minimalism-yet it still fails to account for cognitive load in elderly populations. The font size, contrast ratios, and semantic density are optimized for compliance, not comprehension. I’ve watched my grandmother squint at a bottle of ibuprofen like it’s a quantum physics equation. We need tactile labeling, audio QR codes, and Braille inserts-not just ‘clearer’ text. This isn’t about education; it’s about accessibility as a human right.
Justin Daniel
November 23, 2025 AT 21:48So… you’re telling me I’ve been taking Advil like a caveman for 12 years? 🤦♂️
Turns out ‘take as needed’ doesn’t mean ‘take every time I sneeze.’ Thanks for the reality check. I’m now officially downloading that pill tracker app. And yes, I own three different bottles of acetaminophen. I’m a menace to myself.
Latonya Elarms-Radford
November 24, 2025 AT 03:52Let us not mistake the FDA’s bureaucratic scaffolding for wisdom. The label is not truth-it is a compromise between corporate liability and public health, written by lawyers who have never held a child’s fever syrup in trembling hands. We are taught to trust the label, yet the label is a monument to institutional avoidance. The real tragedy isn’t that people misread it-it’s that we’ve been conditioned to believe reading it is enough. The system is designed to absolve itself, not to heal. And we, the consumers, are the willing acolytes of this liturgy of lethargy.
Mark Williams
November 25, 2025 AT 20:17Key pharmacokinetic variable often overlooked: gastric emptying time modulates bioavailability. Taking doxycycline with dairy? You’re chelating calcium, reducing absorption by up to 50%. ‘Take on empty stomach’ isn’t a suggestion-it’s a pharmacodynamic imperative. Same with levothyroxine. Food, caffeine, even fiber supplements can alter TSH levels. This isn’t ‘common sense’-it’s clinical pharmacology 101. If your pharmacist doesn’t explain this, find a new one.
Ravi Kumar Gupta
November 26, 2025 AT 06:45In India, we don’t have pharmacies handing out syringes. We use the cap. Or a spoon. Or sometimes, the child’s own fingers. I’ve seen mothers give 10 mL of paracetamol using a tea spoon-because ‘it looks right.’ No one has a measuring cup. No one has time. So we pray. And hope. This guide is beautiful. But it’s written for people who have access. What about the village where the nearest pharmacy is 30 km away? We need this in Hindi, Tamil, Bengali-with pictures. Not just words. The label is useless if the reader can’t read.
Rahul Kanakarajan
November 27, 2025 AT 18:36Wow. Another ‘read the label’ lecture. Congrats. You’ve discovered water is wet. Everyone knows you shouldn’t mix alcohol with painkillers. But you know what? Most people don’t care. They’re tired. They’re in pain. They’ve got three kids, a job, and a dog that threw up on the rug. You think they’re gonna pull out a ruler and calculate mL per kg? No. They’re gonna take the pill. And if they die? Well. That’s what happens when you’re poor and tired. This post is performative. It doesn’t fix anything. It just makes the rich feel better about themselves.
Nikhil Chaurasia
November 28, 2025 AT 06:19My uncle took his blood thinner with grapefruit juice for six months because he liked the taste. He ended up in ICU with a GI bleed. No one told him. The label said ‘avoid grapefruit’-but he didn’t know what grapefruit juice meant. He thought it was ‘grapefruit-flavored soda.’ We need visuals. Icons. A little picture of a grapefruit with a red slash. Language fails. Pictures don’t.
ann smith
November 29, 2025 AT 20:02This is so important 💙
Just last week, my mom mixed her blood pressure med with her sleep aid because she thought ‘both make me sleepy’-and she ended up dizzy for hours. I’m printing this out and taping it to her medicine cabinet. Thank you for writing this with so much care. ❤️
Julie Pulvino
December 1, 2025 AT 00:32I used to think ‘take with food’ meant ‘eat something after.’ Turns out, it means ‘eat something BEFORE.’ My stomach’s been screaming at me for years. Now I keep a banana by my meds. Small change. Big difference. Also, I now have a little notebook where I write down every pill I take. It’s dumb. But it’s saved me twice. 🙌
Danny Nicholls
December 1, 2025 AT 23:48OMG YES. I just realized I’ve been taking my antibiotic with coffee 🤯 I thought it was fine because ‘it’s just coffee.’ Now I’m gonna use a syringe for my kid’s amoxicillin. And I’m gonna ask for the Medication Guide next time. Also-why do pharmacies never give out the dang syringes unless you ask?? That’s wild. 🙏