When your doctor or pharmacist gives you advice about your medications, it’s easy to think, "I’ll remember this." But between stress, side effects, and the sheer number of pills you might be taking, memory fails. That’s why writing down exactly what they said isn’t just helpful-it’s essential. Proper documentation protects you, your providers, and your health.
Why Documentation Matters More Than You Think
Medication errors cause about 7,000 deaths in the U.S. every year, according to the Institute of Medicine. A big part of that? Miscommunication or missing records. If you switch doctors, go to the ER, or even just forget what dose you’re on, your notes become your lifeline. They’re not just reminders-they’re legal records. Courts have seen cases where patients lost lawsuits because their provider couldn’t prove they were told about a dangerous interaction. And if you’re on Medicare or Medicaid, incomplete records can mean denied claims.What Exactly Should You Write Down?
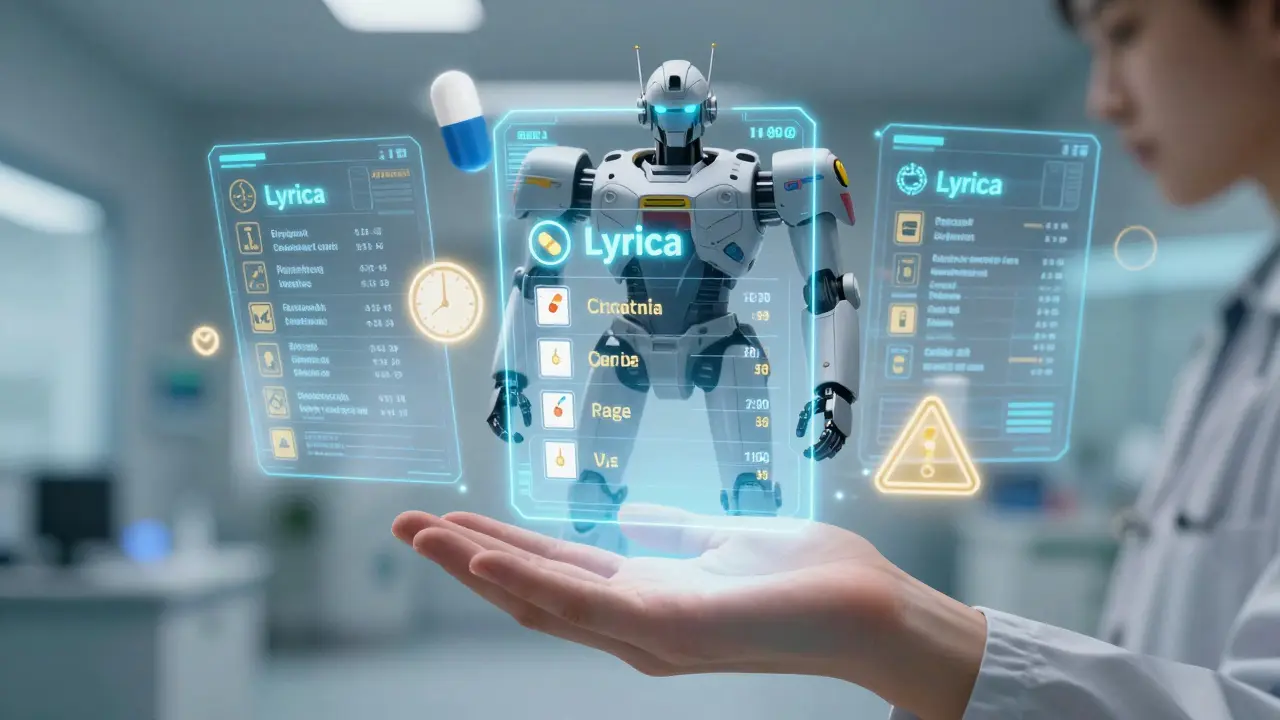
Don’t just scribble "take pill." Be specific. Here’s what to capture every time:- Medication name - Use the brand and generic name. Example: Lyrica (pregabalin)
- Dose and frequency - "Take 75 mg twice daily with food" not "take twice a day"
- Duration - "For 14 days" or "refills: 3"
- Purpose - Why are you taking it? "For nerve pain from diabetes"
- Special instructions - "Do not crush," "avoid alcohol," "take on empty stomach"
- Side effects to watch for - "If you feel dizzy or confused, call your doctor"
- What to do if you miss a dose - "Skip it, don’t double up"
- Follow-up plan - "Return in 2 weeks for blood test"
And don’t forget allergies. Write them down clearly: "Allergic to penicillin-rash and swelling." Include what happened. That’s not optional. It’s a core requirement under NCQA guidelines.
How to Record It So It Actually Helps
There’s a difference between writing something and writing it right.Use a consistent format. Pick one method and stick with it. A notebook, a notes app, or a printable template-it doesn’t matter as long as it’s the same every time. Consistency helps anyone reading it later, including future providers.
Date and sign every entry. If you’re writing this down after your appointment, write the date and your initials. That’s not just good practice-it’s required by the General Medical Council and other regulatory bodies. A note without a date is useless in an emergency.
Don’t rely on memory. If you’re unsure about something, ask again. Say: "Can you repeat that? I want to make sure I get it right." Then write it down right then and there. Providers expect this. They’ve seen patients forget critical details.
Record refusals and noncompliance. If you skip a dose because it made you sick, write that down. If you didn’t fill a prescription because of cost, note it. This isn’t about guilt-it’s about truth. Your next provider needs to know what actually happened, not what was supposed to happen.
Use Technology, But Don’t Trust It Blindly
Eighty-nine percent of U.S. doctors use electronic health records (EHRs) as of 2022. That sounds great-but here’s the catch: your notes in the EHR aren’t always visible to everyone. Your primary care doctor might not see what the pharmacist wrote. The ER won’t have access to your dentist’s notes.That’s why you need your own copy. Use your phone’s notes app. Sync it to the cloud. Take a photo of handwritten notes. Store them in a folder labeled "Medications - [Your Name]." Some apps like Medisafe or MyTherapy let you log meds and share summaries with providers. But don’t assume the system did it for you. Always double-check what’s in your record.
The FDA is pushing for standardized one-page medication guides (PMI) to come with every prescription by 2025. That’s helpful-but it won’t replace personalized advice. Your doctor might say, "Avoid grapefruit with this pill," even if the printed sheet doesn’t mention it. Write that down.
What to Do When You’re Switching Providers
Moving to a new doctor? Bring your documentation. Don’t just say, "I’m on these meds." Hand them a printed list or open your notes on your phone. Include:- All current medications (with doses and reasons)
- Medications you stopped and why
- Allergies and reactions
- Questions you still have
This isn’t extra work-it’s part of your right to continuity of care. The Joint Commission requires medication reconciliation at every transition of care. But they can’t reconcile what isn’t documented. You’re the only one who has the full picture.
Legal Protection Starts With Your Notes
Thirty-eight percent of medical malpractice claims involve medication errors, according to the Physician Insurers Association of America. Many of these happen because there’s no clear record of what was said.Think of your notes like a witness. If you’re ever accused of not following instructions, your written record proves you were trying. If a provider says, "I told you not to take it with alcohol," your note says otherwise. That’s not paranoia-it’s protection.
The American Dental Association says it plainly: "What you write in the record could be read aloud in a court of law." That applies to you too. Your notes are part of your medical history. Treat them like legal documents.
What to Do If Your Provider Won’t Document
Sometimes, providers are rushed. They might say, "I’ll put it in your chart." But if they don’t, you have to step in. Say: "I’d really appreciate it if you could write this down. I want to make sure I’m doing it right."If they refuse or brush you off, write it yourself. Include the date, time, provider’s name, and what was said. You’re not overstepping-you’re ensuring safety. The National Committee for Quality Assurance says patient education must be documented. That includes what you were told, not just what the provider wrote.
Keep It for the Long Haul
Most states require medical records to be kept for 7 to 10 years. Your personal notes should be kept at least that long. Why? Because conditions change. A medication you stopped five years ago might interact with a new one. A past allergy might resurface. Your future self will thank you.Store your notes securely. Use a password-protected digital folder or a locked notebook. Don’t leave them on your desk where a visitor could see them. Privacy matters as much as accuracy.
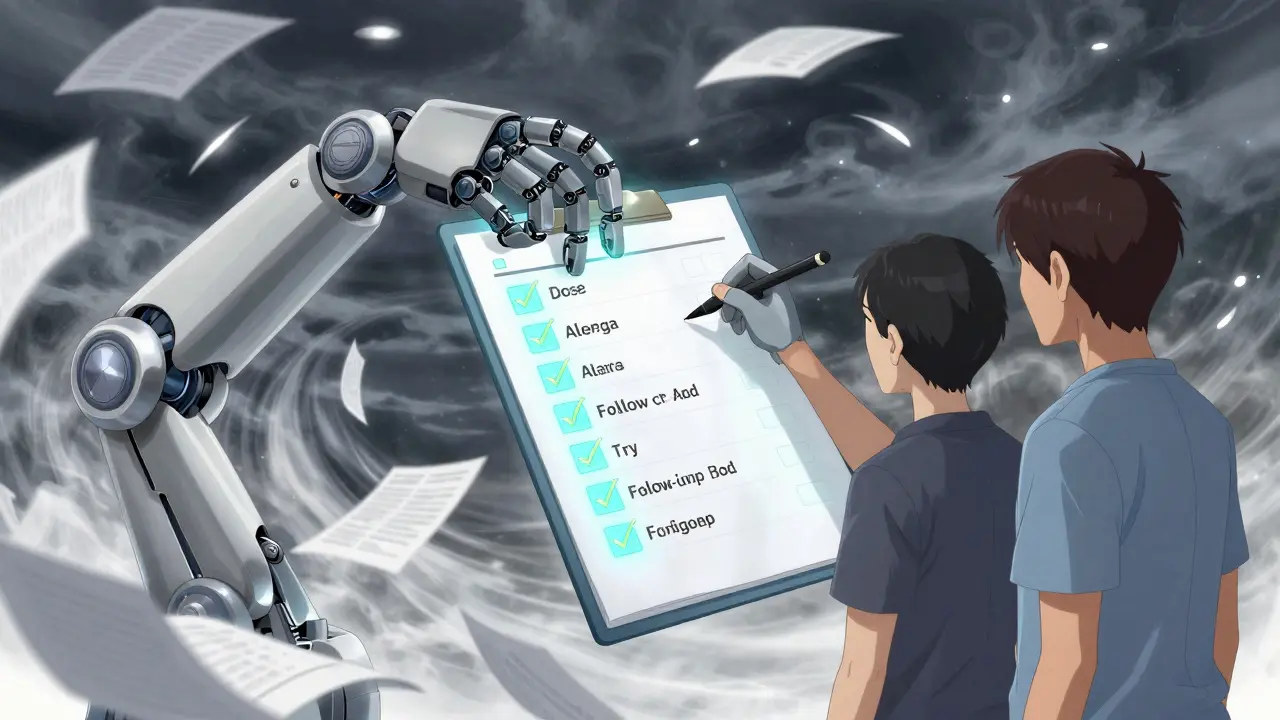
Final Checklist: Did You Cover It All?
Before you leave the office, run through this quick list:- ✅ Medication name (brand and generic)
- ✅ Dose and how often
- ✅ Why you’re taking it
- ✅ Special instructions (food, timing, interactions)
- ✅ Side effects to watch for
- ✅ What to do if you miss a dose
- ✅ Follow-up plan
- ✅ Allergies and reactions
- ✅ Refusals or issues you had
- ✅ Date and your initials
If you checked all 11, you’ve done more than most. You’ve turned advice into action-and that’s how you stay safe.
Do I need to document advice even if my provider says they’ll put it in my chart?
Yes. Provider charts aren’t always complete, timely, or accessible to every caregiver. Your personal record is your backup. It ensures you have accurate, immediate access to the information, especially in emergencies or when switching providers.
What if I don’t understand what the provider said?
Ask them to explain it again-using different words. Say, "Can you explain that like I’m not a doctor?" Then write down what they say. If you’re still unsure, call the pharmacy. Pharmacists are trained to clarify instructions and can confirm dosing, interactions, or side effects.
Can I use my phone’s voice recorder instead of writing?
Voice recordings are better than nothing, but they’re not ideal. You can’t scan them quickly in an emergency. Text is searchable, scannable, and shareable. If you use voice, transcribe the key points into notes afterward. Don’t rely on playback alone.
How do I document advice given over the phone or via telehealth?
Treat phone and telehealth advice the same as in-person visits. Write down the date, time, provider’s name, what was said, and your action plan. The American Dental Association requires this for all communication, even calls received outside office hours. Your record should reflect every interaction that affects your care.
What if I forget to document something right away?
Document it as soon as you can-even hours later. Write "Documentation completed on [date]" to show it’s a follow-up. Don’t wait days. Memory fades. The sooner you write it, the more accurate it will be. And always include the original date of the advice.
Should I share my documentation with my pharmacy?
Yes. Pharmacists are medication experts. Bring your list when you pick up a new prescription. They can spot interactions, refill issues, or errors you might have missed. Many pharmacies now offer medication reviews-ask for one. Your notes make that review more effective.

Alexandra Enns
January 25, 2026 AT 03:38Okay but let’s be real - if your doctor can’t be bothered to write this down properly, they don’t deserve your trust. I had a GP in Toronto who told me to "take it when you feel like it" for my blood pressure med. I wrote it down anyway. Two weeks later, I ended up in the ER. Turns out he didn’t even update his chart. Now I carry a laminated card. No excuses.
Also - why is it always the patient’s job to fix the system? We’re not medical admins. But fine. I’ll keep documenting. Because if I die from a drug interaction, at least my notes will be the only thing that screams "I told you so" to the coroner.
Marie-Pier D.
January 25, 2026 AT 16:16Thank you for this. 🙏 I’m a caregiver for my mom with dementia, and this list saved us so many times. She forgets names, doses, even if she took her pills. Now we have a color-coded notebook: red for antibiotics, green for heart meds, blue for pain. We date every entry and I sign it. She even started doing it herself sometimes - small victories.
Also, I print out a copy for her pharmacy every time we go. They always say "oh, we didn’t have this note!" Like they’re surprised. We’re not asking for a medal. Just don’t kill her.
❤️ You’re doing important work, even if no one says it out loud.
Shanta Blank
January 26, 2026 AT 15:59OH MY GOD I’M SO GLAD SOMEONE FINALLY SAID THIS. My last pharmacist tried to give me a generic version of my antidepressant and I had to pull out my handwritten log with the exact brand name, the date the doctor said "NO GENERIC," and a photo of the scribble with his signature. He looked at me like I was a terrorist with a clipboard.
Turns out he didn’t even know the generic caused seizures in 3% of patients. The label didn’t say that. My doctor did. I wrote it down. He didn’t.
Also - why do people think EHRs are magic? My primary care doctor’s system doesn’t even sync with my psychiatrist’s. I have THREE separate digital folders on my phone. One for each specialist. One for emergencies. One for my sister, who has access in case I OD on benzos again.
PS: I keep a printed copy in my purse. Like a survival kit. With a pen taped to it. I’m not weird. I’m prepared.
Tiffany Wagner
January 26, 2026 AT 17:18i just started doing this after my last dr visit and wow it’s changed everything. i used to forget what i was taking or why. now i have a note called "meds" on my phone. i type it right after the appointment even if i’m tired. i don’t even use capital letters anymore. it’s messy but it’s mine. last week i caught a refill error because i checked my note before picking it up. the pharmacist was like "how did you know?" i just shrugged. now i feel like a superhero. or at least a slightly less confused person.
also i started writing down how i felt after taking things. like "felt foggy after 2pm" or "no anxiety after 3 days". weirdly helpful.
Vatsal Patel
January 27, 2026 AT 05:50Let me guess - you think writing things down makes you special. Like your notebook is a sacred scroll. But here’s the truth: you’re not a doctor. You’re not a lawyer. You’re a person who got scared after one bad experience and now treats every pill like a nuclear launch code.
Doctors aren’t evil. They’re overwhelmed. Your notes don’t change the system. They just make you feel like you’re in control. Which is cute. But it’s not medicine. It’s performance art.
And if you’re really worried about malpractice, maybe stop taking the meds entirely. Less paperwork. Less risk. Just a thought.
Sharon Biggins
January 27, 2026 AT 14:43i just wanted to say thank you for writing this. i’ve been doing this for years since my diagnosis and honestly i thought i was the only one. i use google keep and label everything with the date and dr’s name. sometimes i forget to update it but i try. last month my new dr said "you’ve got the most organized med list i’ve ever seen" and i cried a little. it’s not about being perfect. it’s about not dying alone. you’re not alone in this. we’re all just trying to survive.
ps i still make typos. like "sertraline" becomes "sertraline". but it’s okay. i’m trying.
John McGuirk
January 28, 2026 AT 06:33They’re watching you. They know you’re writing this down. That’s why they push the EHR nonsense - to control the narrative. Your handwritten notes? They can’t edit those. Your phone? It’s not secure. The government, the pharma companies, the insurance bots - they’re all harvesting your data. You think your "meds" folder is private? It’s not. They’re tracking your compliance. Your refusals. Your "side effects" - they’re labeling you as noncompliant before you even leave the clinic.
I keep mine on a burned USB stick. Hidden in my sock drawer. No cloud. No sync. No backup. If they want it, they’ll have to break in. And I’ll be waiting.
Also - your doctor’s name? Don’t write it. Use initials. They’re coming for your records. I’ve seen it happen.
Michael Camilleri
January 30, 2026 AT 03:22Look I’ve been on 17 different meds in 5 years and let me tell you something - if you don’t write it down you’re an idiot. I didn’t write down that my doc told me to stop the gabapentin because I was hallucinating and then I ended up in the psych ward for 3 days because the ER doc thought I was a drug addict. Turns out the hospital had no record of me saying "stop it" because I trusted them. That was the dumbest mistake of my life.
Now I write everything. In crayon if I have to. I even wrote down the nurse’s name who gave me the wrong pill. I don’t care if it’s dramatic. I care if I live.
Also if your provider says "I’ll put it in the chart" they’re lying. They’re busy. They’re tired. They’re paid to move patients through. Not to care. So write it. Or die quietly. Your choice.
lorraine england
January 30, 2026 AT 22:28Love this. I’ve been doing this since my autoimmune flared and I couldn’t remember if I took my steroid that day. Now I have a little green notebook I keep by my coffee maker. I write the date, the med, the dose, and how I felt. Sometimes I draw a little sun if I’m doing okay. A cloud if I’m not.
My sister says I’m obsessive. I say I’m alive. And I showed my new rheumatologist last week - she actually smiled and said "you’re the best patient I’ve had in months."
Also - I started sharing my list with my pharmacy. They’ve caught two errors already. Turns out they appreciate it. Who knew?
Kat Peterson
February 1, 2026 AT 05:31OMG I’M SO GLAD I’M NOT THE ONLY ONE WHO DOES THIS 😭 I have a whole Google Drive folder called "MY MEDICAL LIFE" with 17 subfolders. One for each med. One for side effects. One for doctor scripts. One for pharmacy receipts. One for my emotional breakdowns after each appointment. I even took a selfie with my pill organizer and labeled it "Day 89: Still Alive".
My therapist says I’m a control freak. I say I’m a survivor. And I printed out my entire log on 12 pages and laminated it. I carry it in my purse like a holy text. If I collapse, they’ll know exactly what to do. Or at least what not to give me.
Also - I have a QR code on my necklace that links to it. Yes. I’m that girl. And I don’t care.
Himanshu Singh
February 1, 2026 AT 17:33There’s a quiet dignity in documenting your own healing. We live in a world that treats our bodies like machines to be fixed - not stories to be understood. When you write down what the doctor says, you’re not just keeping track. You’re reclaiming agency. You’re saying: "I am not a case number. I am the keeper of my own truth."
It’s not about fear. It’s about respect. For yourself. For your pain. For the fact that you’re still here, trying.
And yes - your notes matter. Even if no one else reads them. You do. And that’s enough.
🌿
Jamie Hooper
February 3, 2026 AT 02:12mate i just started doing this after my mate nearly died from a drug interaction. i was like "right then" and bought a notebook. i write everything in pencil because i’m always changing my mind. i don’t even bother with dates at first - i just scribble "doc said take this for pain" and then go back later and fix it.
my mum says i’m mad. i say she’s lucky she doesn’t have to remember 14 different pills. i once forgot to write down that i was allergic to penicillin. nearly got a prescription for it. nearly died. now i write it in red. big letters. underlined. twice.
also i keep it in my coat pocket. if i fall over, someone can grab it. simple.
Husain Atther
February 5, 2026 AT 00:05This is a thoughtful and necessary guide. Many patients underestimate the importance of personal documentation, especially in complex chronic conditions. The systemic gaps in healthcare communication are well-documented, and patient-initiated records serve as a vital bridge. Consistency, clarity, and timeliness are indeed the pillars of effective self-advocacy.
I encourage all patients - regardless of health literacy level - to adopt a simple, repeatable system. Even a single sheet of paper with key details can prevent catastrophic errors. The goal is not perfection, but reliability.
Thank you for outlining this with such care.
Helen Leite
February 5, 2026 AT 11:20THEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM. The EHR? It’s a trap. The pills? They’re laced with tracking chips. I saw it on a documentary. Your notes? They’re being scanned. Your handwriting? Analyzed for stress levels. Your phone app? Connected to the NSA. I have a notebook. I write everything. I don’t use electronics. I use pen and paper. I bury it under my garden. In a tin can. With a dead battery inside. They can’t hack dirt.
Also - I don’t trust doctors. I trust my notes. And my notes don’t lie.
👁️🩹