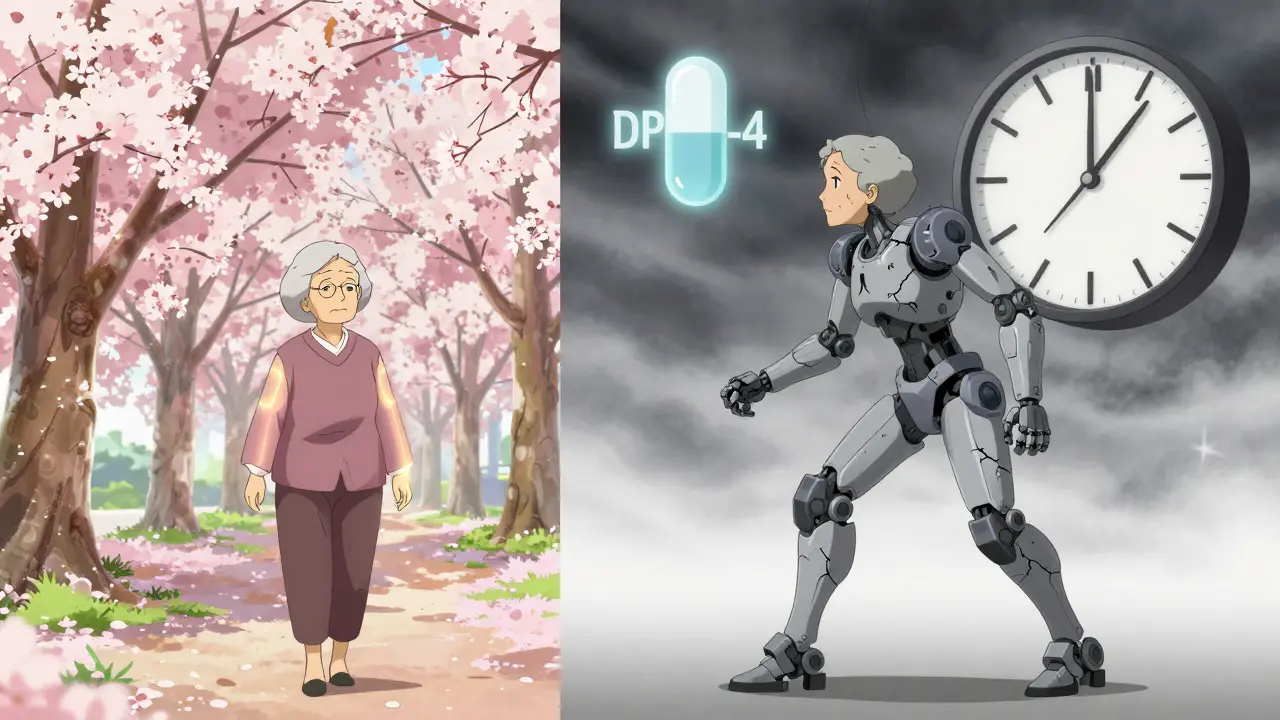
If you’re taking a DPP-4 inhibitor for type 2 diabetes and suddenly notice your knees, hips, or hands start hurting like never before, don’t brush it off as aging or overuse. That pain could be linked to your medication. Since 2015, the FDA has warned that these commonly prescribed diabetes drugs - including sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta), and alogliptin (Nesina) - can cause severe, disabling joint pain in some people. It’s not common, but when it happens, it can turn your life upside down.
What Are DPP-4 Inhibitors and How Do They Work?
DPP-4 inhibitors are oral medications used to lower blood sugar in people with type 2 diabetes. They work by blocking an enzyme called dipeptidyl peptidase-4, which breaks down incretin hormones. These hormones help your body release more insulin after meals and reduce the amount of glucose your liver releases. The result? Better blood sugar control without causing major weight gain or frequent low blood sugar episodes - which is why doctors still prescribe them widely.
Since the first one, sitagliptin, hit the market in 2006, millions of prescriptions have been filled. Even today, with generics available, sitagliptin alone accounts for over 35 million U.S. prescriptions annually. That’s a lot of people relying on these drugs. But behind the numbers are real stories - like the 58-year-old woman who developed crippling knee pain three weeks after starting sitagliptin. Her pain vanished within two weeks of stopping it… and came right back when she accidentally took it again.
The FDA Warning: Severe Joint Pain Is Real
In August 2015, the FDA issued a safety alert after reviewing over 30 cases of severe joint pain linked to DPP-4 inhibitors. They didn’t find just a few odd reports - they found a pattern. Of the 33 confirmed cases in their database:
- 28 were tied to sitagliptin
- 5 to saxagliptin
- 2 to linagliptin
- 1 to alogliptin
- 2 to vildagliptin
Five of those patients had joint pain with more than one DPP-4 inhibitor - a strong clue this isn’t just bad luck with one drug. It’s likely a class-wide effect.
The pain wasn’t mild. All 33 patients said it was severe enough to cut back on daily activities. Ten needed hospital care. Some couldn’t walk. Others lost their jobs. And here’s the kicker: 23 of them got better within a month of stopping the drug. Eight had the pain return when they restarted it. That’s not coincidence - that’s causation.
When Does the Pain Start?
Many assume side effects show up right away. Not with this one. In 22 of the 33 cases, joint pain began within a month of starting the medication. But in others? It took six months. A year. One patient developed severe pain after two years on sitagliptin.
This delay is why so many people get misdiagnosed. Doctors check for arthritis, lupus, gout - anything but the medication they prescribed. Patients end up seeing rheumatologists, getting MRIs, even starting immune-suppressing drugs before someone finally asks: “When did you start this diabetes pill?”
The FDA says: “Consider DPP-4 inhibitors as a possible cause even if you’ve been taking them for a long time.” Don’t assume it’s just aging. Don’t assume it’s unrelated. If your joint pain is new, unexplained, and worsening - look back at your meds.

How Common Is This Side Effect?
Let’s put this in perspective. Over 30 million prescriptions are filled each year in the U.S. alone. Only 33 confirmed cases of severe joint pain were reported to the FDA between 2006 and 2013. That’s less than 0.0001%. So yes - it’s rare.
But rare doesn’t mean imaginary. And it doesn’t mean it won’t happen to you. In clinical trials, 5-10% of people reported mild joint discomfort. That’s different from the disabling pain the FDA documented. Mild ache? Maybe just a side effect. Sharp, constant, movement-limiting pain? That’s a red flag.
Some studies back this up. A 2021 analysis of U.S. health records found DPP-4 inhibitor users had a 24% higher risk of needing medical care for joint pain compared to users of other diabetes drugs. Other studies, like one in Taiwan, found no link - but they relied on hospital coding systems that often miss subtle or non-hospitalized cases.
The bottom line? The risk is low, but the impact is high. And when it happens, it’s serious.
What Should You Do If You Feel This Pain?
Don’t stop your medication on your own. That could spike your blood sugar and put you at risk for complications. But don’t ignore it either.
Here’s what to do:
- Call your doctor. Don’t wait. Say: “I’ve had new, severe joint pain since starting [medication name].”
- Track your symptoms. Note which joints hurt, how bad it is (1-10 scale), when it started, and whether it’s getting worse.
- Don’t assume it’s arthritis. Tell your doctor about your medication. Many don’t make the connection unless you do.
- Ask about stopping the drug. If your doctor agrees, stopping the DPP-4 inhibitor is often the fastest way to relief. Most patients improve within days to weeks.
- Don’t restart it. If the pain went away and came back after restarting - that’s your answer. Avoid rechallenge.
Some patients report feeling better within 48 hours of stopping. Others take a month. But almost everyone gets better - if they stop the drug.
What Are the Alternatives?
If you need to stop a DPP-4 inhibitor, your doctor has other options. Metformin is still first-line for most people. GLP-1 receptor agonists like semaglutide (Ozempic) are more effective for weight loss and blood sugar control. SGLT2 inhibitors like empagliflozin (Jardiance) help with heart and kidney protection. Sulfonylureas and insulin are older but still useful, though they carry higher risks of low blood sugar and weight gain.
Your choice depends on your health goals: weight loss? Heart protection? Simplicity? Cost? Talk to your doctor about what fits your life - not just your lab numbers.
Other Side Effects to Watch For
DPP-4 inhibitors are generally well-tolerated. But besides joint pain, there are other red flags:
- Pancreatitis: Severe abdominal pain, nausea, vomiting. Call your doctor immediately.
- Allergic reactions: Swelling of the face, lips, tongue, or throat. Trouble breathing. This is an emergency.
- Bullous pemphigoid: Large, fluid-filled blisters on the skin. Can require hospitalization.
- Hypoglycemia: More likely if you’re also taking sulfonylureas or insulin.
If you develop any of these, don’t wait. Contact your doctor right away.
Final Thoughts: Know the Signs, Speak Up
DPP-4 inhibitors are safe and effective for most people with type 2 diabetes. But no drug is perfect. The FDA’s warning isn’t about fear - it’s about awareness. You’re not being paranoid if you notice pain and wonder if it’s your pill. You’re being smart.
Millions take these drugs without issue. But for the few who do develop severe joint pain, the difference between early detection and delayed diagnosis is weeks of agony - or a quick return to normal life.
If you’re on one of these medications and feel new, unexplained joint pain - especially if it’s severe - talk to your doctor. Don’t wait. Don’t assume it’s nothing. Your body is trying to tell you something.
Can DPP-4 inhibitors cause joint pain even after years of use?
Yes. While many cases of joint pain start within the first month of taking a DPP-4 inhibitor, some patients develop symptoms after six months or even longer. The FDA specifically warns that this side effect can occur at any time during treatment, even after years of use. If you’ve been on the medication for a long time and suddenly develop severe joint pain, it’s still worth considering the drug as a possible cause.
Will my joint pain go away if I stop the medication?
In most cases, yes. Of the 33 confirmed cases reviewed by the FDA, 23 patients saw their joint pain resolve within one month of stopping the DPP-4 inhibitor. For many, improvement began within days. However, if you restart the medication, the pain often returns - sometimes within 48 hours. This pattern strongly supports a direct link between the drug and the symptom.
Are all DPP-4 inhibitors equally likely to cause joint pain?
The FDA’s analysis suggests this side effect may affect the entire class, not just one drug. While sitagliptin had the most reported cases (28), joint pain was also linked to saxagliptin, linagliptin, alogliptin, and vildagliptin. Five patients experienced the pain with more than one DPP-4 inhibitor, indicating a possible class-wide mechanism. So if you’ve had joint pain with one, switching to another may not help.
How is DPP-4 inhibitor-induced joint pain different from arthritis?
Unlike rheumatoid arthritis or osteoarthritis, DPP-4 inhibitor-related joint pain typically doesn’t show up on X-rays or blood tests. There’s no joint swelling, redness, or elevated inflammatory markers in most cases. The pain is often described as deep, constant, and disabling - affecting multiple joints symmetrically - and improves rapidly after stopping the drug. If your joint pain appears suddenly, isn’t linked to injury or aging, and improves after stopping your diabetes pill, this could be the cause.
Should I stop taking my DPP-4 inhibitor if I have mild joint discomfort?
Not necessarily. Mild joint discomfort - like occasional stiffness or a dull ache - is reported by 5-10% of users in clinical trials and is often not serious. Only severe, disabling pain that limits your daily activities is linked to the FDA warning. If your pain is mild and doesn’t interfere with walking, working, or sleeping, talk to your doctor before making any changes. But if it’s worsening or becoming unbearable, don’t wait - contact your provider.


Stewart Smith
January 1, 2026 AT 09:03So I’ve been on Januvia for 3 years and my knees have been acting up since last winter. Thought I was just getting old or maybe I needed new sneakers. Turns out? Could be the pill. I called my doc yesterday and we’re switching me off it. Felt like a dumbass for not connecting the dots sooner.
Retha Dungga
January 2, 2026 AT 05:40bro this is wild 🤯 i was like ‘why do my hips hurt when i stand up’ and now i realize it’s not my yoga routine… it’s the diabetes pill i’ve been taking like it’s vitamin gummies 😅 maybe we all need to stop treating meds like magic beans
Jenny Salmingo
January 3, 2026 AT 11:20My mom had this happen. She was in so much pain she couldn’t garden. Doctor said it was arthritis. She cried. Then she stopped the medicine and two weeks later she was planting tomatoes again. Don’t ignore your body. It talks. You just gotta listen.
Aaron Bales
January 3, 2026 AT 15:15If you’re on a DPP-4 inhibitor and have new, unexplained joint pain, tell your doctor immediately. Don’t wait. Don’t assume it’s aging. Document it. Track it. Be the patient who speaks up. It’s not paranoia - it’s responsibility.
Lawver Stanton
January 4, 2026 AT 13:56Okay but let’s be real - how many people are just blindly popping these pills like candy? I mean, you get diagnosed with type 2 diabetes and suddenly you’re handed a whole pharmacy catalog and told ‘take one of these, maybe this one, or if you’re lucky, this one with the pretty blue capsule.’ Nobody says ‘hey, this might make your joints feel like they’re being crushed by a troll.’ And then when you start hurting, you blame your yoga mat or your cat jumping on your knee. Meanwhile, your doctor’s still stuck in 2010 thinking ‘oh, it’s just inflammation.’ Bro, it’s been 15 years since Januvia came out. We should know better. And yet here we are. Millions of prescriptions. Zero real warnings on the bottle. Just a footnote buried in the 87-page insert you never read because you’re too busy Googling ‘why does my knee sound like popcorn’ at 2 a.m.
Sara Stinnett
January 4, 2026 AT 18:35How predictable. Another pharmaceutical miracle weaponized by profit-driven indifference. We celebrate ‘breakthroughs’ while ignoring the quiet suffering of those who don’t fit the clinical trial demographic. The FDA’s ‘33 cases’ is a farce - it’s the tip of an iceberg built on passive surveillance, underreporting, and the institutional dismissal of patient testimony. This isn’t a side effect - it’s a systemic failure masked as pharmacology. And yet, we still treat these drugs like gospel because convenience trumps conscience. Wake up.
linda permata sari
January 6, 2026 AT 16:40I’m from Indonesia and my cousin in Jakarta took linagliptin for 18 months and started having knee pain like fire. No swelling. No redness. Just… pain. No one believed her until she stopped it. Now she’s on metformin and dancing again. This isn’t just an American thing. It’s everywhere.
Brandon Boyd
January 8, 2026 AT 01:11You got this. If you’re reading this and you’re on one of these meds and you’ve been feeling off - don’t wait. Don’t feel guilty. Your health isn’t a second thought. Call your doctor today. Write down your symptoms. Bring this post. You’re not overreacting - you’re being the hero of your own story. And if you’ve already stopped the drug and feel better? Celebrate. You listened to your body. That’s power.