Drug Selection Guide
Find Your Best Medication Option
Select your medical situation to see which drug is most appropriate based on the article content.
Results
Select a situation and click "Find Best Option" to see recommendations.
When you hear the name Cytotec is a misoprostol tablet that mimics prostaglandins to trigger uterine contractions or protect the stomach lining, it often feels like the only tool for induction or medical abortion. Yet doctors and patients have several other options, each with its own strengths, costs, and side‑effects. Below you’ll find a plain‑spoken walk‑through of how Cytotec stacks up against the most common alternatives so you can decide which drug fits your situation best.
How Misoprostol Works
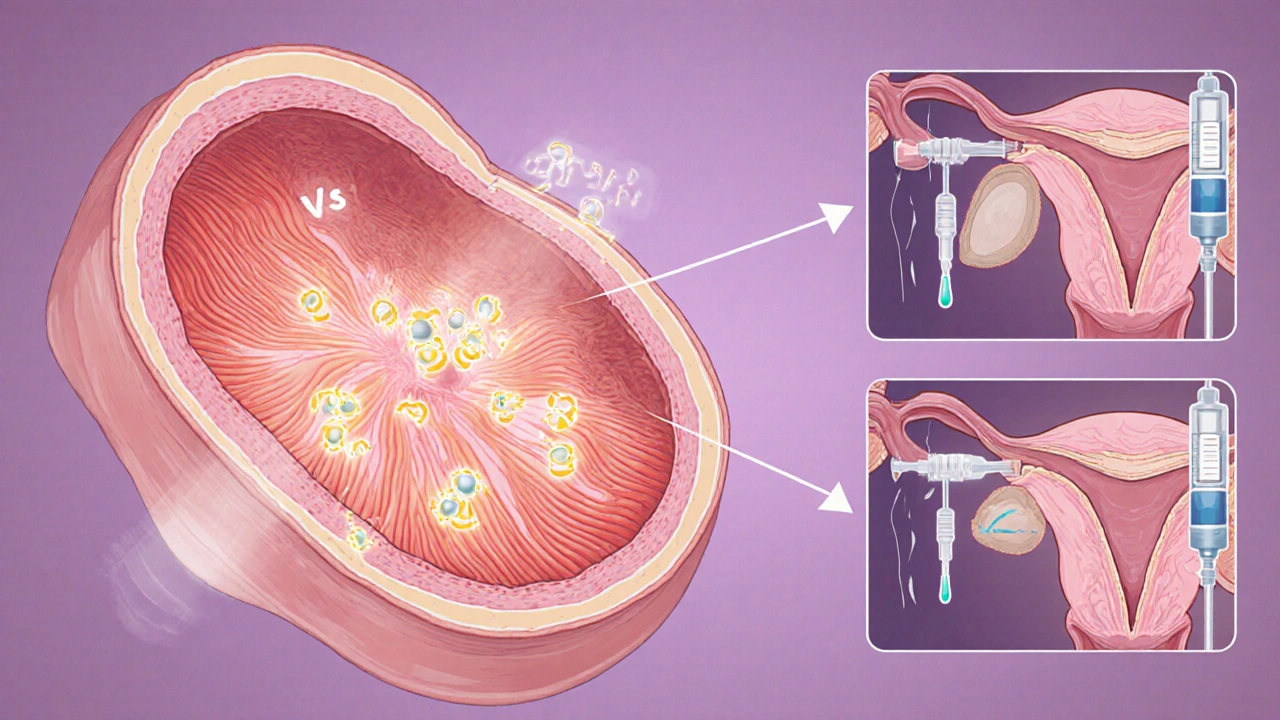
Misoprostol belongs to the prostaglandin E1 family. It binds to uterine receptors, causing the muscle to contract and the cervix to soften. At lower doses it also reduces stomach acid, which is why it’s marketed for ulcer prevention.
Typical Clinical Uses
- Labor induction in late‑term pregnancy.
- Medical termination of early pregnancy (often paired with Mifepristone).
- Treatment of postpartum hemorrhage.
- Gastric ulcer prophylaxis for patients taking NSAIDs.
Main Alternatives Overview
Below are the drugs you’ll most likely encounter when Cytotec isn’t the first choice.
- Dinoprostone - a synthetic prostaglandinE2 used primarily for cervical ripening.
- Carboprost Tromethamine - a prostaglandinF2α analogue, best known for controlling postpartum bleeding.
- Oxytocin - a hormone that stimulates uterine contractions; the go‑to for active labor.
- Mifepristone - a progesterone antagonist that prepares the uterus for misoprostol‑induced abortion.
- Omeprazole - a proton‑pump inhibitor used for ulcer prevention, offering a non‑prostaglandin route.
- Lansoprazole - another PPI, similar to omeprazole but often cheaper in bulk.
- Ranitidine - an H2‑blocker that lowers stomach acid; still prescribed where PPIs aren’t covered.
Side‑by‑Side Comparison
| Drug | Class | Typical Dose | Primary Indication | Onset (minutes) | Route | Approx. Cost (AUD) |
|---|---|---|---|---|---|---|
| Cytotec (Misoprostol) | ProstaglandinE1 analog | 200µg‑800µg every 3‑4h | Labor induction, medical abortion, ulcer prophylaxis | 15‑30 (uterine), 30‑60 (GI) | Oral, sublingual, vaginal | $2‑$4 per tablet |
| Dinoprostone | ProstaglandinE2 analog | 0.5‑3mg vaginal insert | Cervical ripening, induction | 30‑60 | Vaginal, intra‑uterine | $30‑$45 per dose |
| Carboprost Tromethamine | ProstaglandinF2α analog | 250µg IM every 15‑90min (max 2mg) | Post‑partum hemorrhage | 10‑15 | IM injection | $80‑$120 per vial |
| Oxytocin | Peptide hormone | 2‑10IU IV infusion | Active labor, post‑partum bleeding | 1‑2 | IV/IM | $5‑$10 per vial |
| Mifepristone + Misoprostol | Progesterone antagonist + prostaglandin | 200mg mifepristone oral then 800µg misoprostol 24‑48h later | Early medical abortion (≤9weeks) | 24‑48h after mifepristone | Oral (both) | $50‑$70 total |
| Omeprazole | Proton‑pump inhibitor | 20‑40mg daily | Ulcer prevention/treatment | 30‑60 | Oral | $1‑$2 per tablet |
| Lansoprazole | Proton‑pump inhibitor | 15‑30mg daily | Ulcer prevention/treatment | 30‑60 | Oral | $0.80‑$1.50 per tablet |
| Ranitidine | H2‑blocker | 150‑300mg twice daily | Acid‑related disorders | 45‑75 | Oral | $0.30‑$0.60 per tablet |
Choosing the Right Option
Think of drug selection as matching a tool to a job. Here’s a quick decision guide:
- Need rapid uterine contraction for postpartum bleeding? Carboprost or Oxytocin are usually first‑line; misoprostol works but may be slower.
- Planning induction at 39weeks without a cervical score? Dinoprostone gives gentle ripening; misoprostol is cheaper and can be used at home but may cause more intense contractions.
- Early medical abortion (up to 9weeks)? The combination of Mifepristone + Misoprostol is the gold standard; using Cytotec alone is possible but slightly less effective.
- Protecting the stomach while on NSAIDs? Proton‑pump inhibitors like Omeprazole are now preferred in many guidelines for their stronger acid suppression versus misoprostol’s ulcer protection.
Safety, Side‑Effects, and Contra‑Indications
All drugs carry risks; the key is knowing which ones matter most for you.
- Cytotec (Misoprostol): Nausea, diarrhoea, cramping, fever. Not for women with previous cesarean scar in labor.
- Dinoprostone: Vaginal irritation, uterine hyperstimulation. Requires storage at2‑8°C.
- Carboprost: High fever, bronchospasm, especially in asthmatics - use cautiously.
- Oxytocin: Water‑intoxication if infused too fast, fetal distress from hyperstimulation.
- PPIs (Omeprazole/Lansoprazole): Long‑term use linked to low magnesium, higher infection risk; short courses are safe.
- Ranitidine: Rare liver issues; many brands recalled in 2024, so availability varies.
Cost & Accessibility in Australia (2025)
Pricing can sway decisions, especially when Medicare or private health cover is involved.
- Misoprostol tablets are subsidised under PBS for ulcer prevention - about $2 per pack.
- Dinoprostone gels are not PBS‑listed; you’ll pay out‑of‑pocket, roughly $40‑$60 per dose.
- Carboprost is stocked in hospitals only; cost passed to the patient via hospital fees.
- Oxytocin is widely available in clinics; a vial costs under $10.
- Omeprazole and Lansoprazole are both PBS‑listed for chronic ulcer disease; prices $0.90‑$1.30 per tablet.
Bottom Line
If you need a low‑cost, versatile drug for both obstetric and GI uses, Misoprostol alternatives should be weighed against the specific outcome you’re after. For precise cervical ripening, Dinoprostone takes the lead; for rapid control of bleeding, Carboprost or Oxytocin are safer bets; and for ulcer protection, modern PPIs have largely supplanted misoprostol in most guidelines.
Frequently Asked Questions
Can I use Cytotec at home for labor induction?
Many clinicians prescribe low‑dose misoprostol for home use, but you need a clear protocol and a way to contact your midwife or doctor if contractions become too strong.
Is Dinoprostone safer than Misoprostol for first‑time mothers?
Dinoprostone causes slower, more controlled cervical softening, which many providers prefer for first‑timers. Misoprostol works faster but can cause more intense cramps.
What’s the best drug for postpartum hemorrhage?
Carboprost is the go‑to when oxytocin alone doesn’t stop bleeding. It’s given by injection and acts quickly, but avoid it in asthmatic patients.
Are PPIs really needed if I’m already taking Misoprostol for ulcer prevention?
Current Australian guidelines suggest PPIs provide stronger acid suppression and are preferred for long‑term NSAID users. Misoprostol remains an option when PPIs are unavailable or contraindicated.
How much does a typical course of Mifepristone+Misoprostol cost?
In 2025, the combined regimen costs around $50‑$70 in Australian pharmacies, often covered partially by private health insurance.

Xing yu Tao
October 15, 2025 AT 13:23In contemplating the pharmacologic landscape presented, one discerns a pattern wherein cost, efficacy, and safety intersect in a delicate equilibrium. Cytotec, with its versatile applications, exemplifies the principle of multifunctionality that is prized in therapeutic design. Yet, the alternatives delineated-Dinoprostone, Carboprost, Oxytocin, and the various PPIs-serve as pertinent reminders that no singular agent can universally satisfy every clinical nuance. The comparison table, therefore, operates not merely as a ledger of numbers but as a conceptual framework for judicious decision‑making. Ultimately, the clinician’s discernment, guided by patient‑specific factors, will determine the optimal selection.
Adam Stewart
October 15, 2025 AT 15:36Consider the patient’s prior obstetric history when weighing misoprostol against the other options.
Selena Justin
October 15, 2025 AT 17:50It is helpful to note that while misoprostol is cost‑effective, the onset of action can be more abrupt compared with dinoprostone, which may be preferable for first‑time mothers seeking a gentler cervical ripening. Additionally, for those with asthma, carboprost’s bronchospastic potential warrants caution, making oxytocin a safer default for postpartum hemorrhage. The ulcer‑prevention segment also benefits from the stronger acid suppression offered by PPIs, aligning with current Australian guidelines.
felix rochas
October 15, 2025 AT 20:03What they don’t tell you is that the pharmaceutical lobby has engineered these “alternatives” to keep misoprostol out of the market!!! They push expensive PPIs and obscure the fact that Cytotec works just as well!! Beware of hidden corporate agendas!!!
inder kahlon
October 15, 2025 AT 22:16From a pharmacokinetic standpoint, misoprostol’s rapid absorption via the vaginal route accounts for its quicker uterine response, whereas dinoprostone’s gel formulation introduces a latency that can be beneficial for controlled induction. The cost differential is also stark, with Cytotec at a few dollars per dose versus dinoprostone’s tens of dollars.
Dheeraj Mehta
October 16, 2025 AT 00:30👍 The affordability of Cytotec really shines in low‑resource settings, and its versatility means fewer pills to stock. Keep in mind the side‑effect profile is manageable with proper counseling.
Kyle Salisbury
October 16, 2025 AT 02:43In many Commonwealth countries, the practice patterns favor oxytocin for active labor, reflecting both historical training and drug availability. Yet, the growing body of evidence from Asia shows a resurgence of misoprostol use for home‑based inductions, underscoring cultural shifts in obstetric care. Awareness of these regional differences can guide clinicians when consulting expatriate patients.
Angie Robinson
October 16, 2025 AT 04:56The data presented glosses over the real‑world failures of misoprostol in high‑risk pregnancies; the authors cherry‑pick studies that paint it in a favorable light. A critical reader should demand more robust comparative trials before accepting these conclusions.
Emmons Kimery
October 16, 2025 AT 07:10🗣️ While it’s true that misoprostol isn’t perfect, many providers have reported satisfactory outcomes when protocols are strictly followed. It’s also worth noting that the side‑effects are often transient and can be mitigated with anti‑emetics. Let’s keep the conversation evidence‑based and supportive of patient autonomy.
Mimi Saki
October 16, 2025 AT 09:23😊 Ultimately, the choice lies with the patient after a thorough discussion of benefits and risks, and a shared decision‑making approach empowers them to feel confident in their care.
Subramaniam Sankaranarayanan
October 16, 2025 AT 11:36First, it must be emphasized that the ethical dimension of prescribing misoprostol extends beyond mere cost considerations; it implicates the principle of justice in healthcare distribution. When a drug like Cytotec can be procured for a fraction of the price of proprietary alternatives, denying its use to economically disadvantaged populations becomes a moral failing. Second, the pharmacodynamic profile reveals that misoprostol, by virtue of its prostaglandin E1 analog structure, offers a unique dual benefit: uterine contraction and gastric mucosal protection, a combination not replicated by the other agents listed. Third, the table’s omission of patient‑centered outcomes-such as satisfaction scores and quality‑of‑life measures-limits its applicability in real‑world settings. Fourth, the authors fail to discuss the regulatory landscape, where misoprostol’s off‑label status in some jurisdictions may introduce legal complexities for clinicians. Fifth, while dinoprostone’s controlled release is advantageous for slow ripening, it also carries a higher risk of hyperstimulation, which can jeopardize fetal well‑being. Sixth, carboprost’s contraindication in asthmatics is not a trivial footnote; it demands vigilant screening, which may be impractical in resource‑limited environments. Seventh, oxytocin’s rapid onset is ideal for active labor, yet its potential for water‑intoxication necessitates careful fluid balance monitoring. Eighth, the discussion of PPIs neglects the emerging data linking long‑term proton‑pump inhibition to micronutrient deficiencies and altered gut microbiota, issues that must be weighed against misoprostol’s side‑effect profile. Ninth, the price comparisons, while useful, do not account for indirect costs such as administration equipment for injectable agents like carboprost. Tenth, the therapeutic hierarchy presented implicitly suggests that misoprostol should be the default, but this overlooks patient preferences for route of administration, which can vary widely. Eleventh, the safety data cited are predominantly from controlled trial environments, and real‑world adverse event rates may differ. Twelfth, the authors omit a discussion of training requirements; misuse of misoprostol can lead to uterine rupture in scarred uteri, underscoring the need for adequate clinician education. Thirteenth, the overall tone of the article appears to advocate for misoprostol without sufficient acknowledgment of its limitations, which is a form of bias. Fourteenth, from a public health perspective, promoting a low‑cost, widely available drug aligns with the goals of reducing maternal morbidity in underserved regions. Finally, the holistic appraisal of evidence demands that we balance efficacy, safety, cost, and ethical imperatives, rather than privileging any single dimension.
Kylie Holmes
October 16, 2025 AT 13:50Great synthesis! Your point about justice reminds us that affordability isn’t just an economic metric but a moral imperative. I also appreciate the call for better training-without proper protocols, even the best drug can cause harm. Let’s champion both evidence and equity in our prescribing habits.
Jennifer Wees-Schkade
October 16, 2025 AT 16:03Enough talk; prescribe the cheapest effective drug now.