Every year, more than 100,000 children die from pneumonia because the medicine they were given had no active ingredient. This isn’t a statistic from decades ago-it’s happening right now, in 2025, in villages across Africa, South Asia, and Latin America. The medicine looked real. The packaging was perfect. The pharmacy seemed legitimate. But the pills were empty. Or worse-they contained toxic chemicals that poisoned the body instead of healing it.
What Exactly Are Counterfeit Drugs?
Counterfeit drugs aren’t just knock-offs like fake sneakers or handbags. They’re life-or-death frauds. The World Health Organization breaks them into two types: substandard and falsified. Substandard drugs are made by legitimate companies but fail quality checks-maybe they expired, were stored wrong, or were diluted during transport. Falsified drugs are outright fakes: made in secret labs, often in China or Bangladesh, with no regard for safety, purity, or effectiveness. These fake medicines can contain:- No active ingredient at all (about 30% of cases)
- Too little active ingredient (45% of cases)-enough to make you feel slightly better, but not enough to kill the infection
- Wrong ingredients-like rat poison, paint thinner, or industrial chemicals (25% of cases)
Why Are Developing Nations So Affected?
It’s not because people in these countries are careless. It’s because the system is broken. In many low-income countries, a single dose of a real antimalarial drug can cost $10-more than a day’s wage. Counterfeit versions? They sell for $1 or less. When you’re starving, choosing the cheaper option isn’t a luxury-it’s survival. But here’s the cruel twist: the fake drugs don’t just save money-they steal lives. A 2022 Lancet study found that 87% of counterfeit antibiotics in developing nations contained too little active ingredient to treat infections. That means a child given fake amoxicillin for pneumonia doesn’t just get sicker-they develop drug-resistant strains of bacteria. And those strains don’t stay in one village. They spread globally. Weak regulation makes it worse. In many countries, medicine regulators are underfunded, understaffed, and lack the tools to test drugs. A spectroscopy machine that can detect fake pills with 95% accuracy costs $50,000. Most rural clinics can’t afford one. Even if they could, 60% of them don’t have reliable electricity to run it.The Human Cost: Real Stories, Real Deaths
In 2012, over 200 people died in Lahore, Pakistan, after being given heart medication that contained lethal levels of a toxic chemical. The drugs had been distributed through public hospitals. Families didn’t know the pills were fake until it was too late. A mother in Nigeria posted on Reddit in March 2025: “My brother died of malaria last year after taking counterfeit Coartem. The pharmacy had no way to verify authenticity.” She didn’t even know what counterfeit meant. She just knew her brother took the pills, got worse, and didn’t wake up. In Kenya, healthcare workers found that 50% of malaria test kits in rural clinics were fake. That means patients were being misdiagnosed-given malaria drugs when they had typhoid, or vice versa. Misdiagnosis leads to death. And the cycle continues. In Ghana, a woman used the mPedigree SMS verification system to check her antimalarial pills. The system replied: “This batch is fake.” She returned to the pharmacy and reported it. Later, she learned that three other families in her village had bought the same batch. One child died. Her child lived.
How Do Fake Drugs Get Into the System?
Counterfeit drugs don’t appear out of nowhere. They travel through long, hidden supply chains. A fake pill might be made in a basement lab in Guangdong, China. Then shipped to a warehouse in Lebanon. From there, it’s repackaged and sent to a distributor in Nigeria. Then sold through a local pharmacy, a street vendor, or even a mobile clinic. Each stop adds layers of opacity. By the time it reaches the patient, no one knows where it came from. Online pharmacies make it worse. In Southeast Asia, 68% of negative reviews on Trustpilot mention suspected counterfeit drugs. People complain that pills “dissolved in water when they shouldn’t” or that “nothing happened after taking them.” But most buyers don’t know how to verify legitimacy. They trust the website, the price, the packaging. Criminals now use 3D printing to replicate packaging with 99% accuracy. Even pharmacists can’t tell the difference without lab equipment. And because the drugs are sold across borders, law enforcement struggles to track them. Interpol’s 2025 Operation Pangea XVI shut down 13,000 websites and arrested 769 suspects-but for every bust, ten more pop up.What’s Being Done?
Some solutions are working. The WHO’s Global Digital Health Verification Platform, launched in March 2025, uses blockchain to track every pill from factory to patient. It’s already active in 27 countries. If a drug is scanned and flagged as fake, the system alerts regulators and warns consumers. In Ghana, the mPedigree system lets people text a code from the pill pack to a free number. Within seconds, they get a reply: “Authentic” or “Fake.” It costs nothing. It works on any phone-even old flip phones. Over 15,000 people have used it. It saved lives. Solar-powered testing kits are now being rolled out in rural clinics. They cost under $200, run on sunlight, and give results in 10 minutes. In 12 African countries, they’ve improved detection rates by 70%. But progress is slow. Only 22% of pharmacies in low-income countries use any kind of verification system. In high-income countries, it’s 98%. The gap isn’t just about money-it’s about willpower. Many governments still treat counterfeit drugs as a criminal issue, not a public health emergency.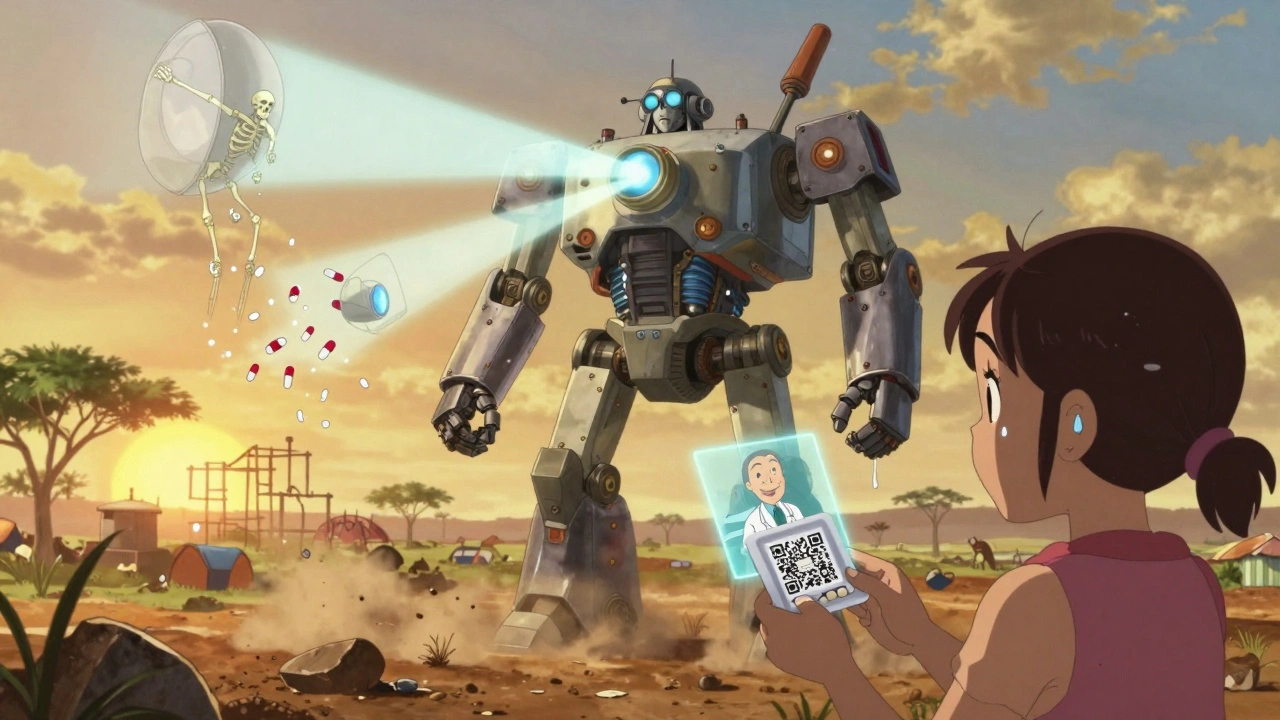
What Can Be Done?
The solution isn’t just better tech-it’s better systems. Here’s what needs to happen:- Strengthen local regulators. Countries need trained inspectors, testing labs, and legal power to shut down fake drug operations.
- Make real drugs affordable. If genuine antimalarials cost less than $0.50 per dose, people won’t risk buying fakes.
- Train community health workers. In villages where no pharmacy exists, a trained nurse can spot fake pills by texture, color, or smell-with 70% accuracy after 40 hours of training.
- Use simple verification tools. SMS, QR codes, and voice-based systems work better than apps that require smartphones or literacy.
- Hold global supply chains accountable. Every country that exports medicines must verify their quality before shipping. No exceptions.
What You Can Do
If you live in a high-income country, you might think this doesn’t affect you. But it does. Drug-resistant infections born from fake medicines in Africa or India can spread to your city. The next pandemic might start with a fake antibiotic. You can support organizations like Doctors Without Borders, the WHO, or mPedigree. Donate to their verification programs. Advocate for policies that tie international aid to medicine quality. Pressure pharmaceutical companies to make their drugs affordable in low-income markets. If you’re traveling to a developing country, never buy medicine on the street. Even if it looks real, it might not be. Use only licensed pharmacies. Ask for the batch number and verify it if possible.The Future Is Not Set in Stone
The World Bank warns that without major intervention, counterfeit drugs could cause 5.7 million deaths in developing nations by 2030. But that’s not inevitable. AI-powered detection systems, solar testing kits, and community-led verification are already proving they work. The technology exists. The knowledge exists. What’s missing is the global will to act. This isn’t about charity. It’s about justice. People deserve medicine that works. No matter where they live. No matter how much they earn. Fake drugs aren’t a business-they’re a crime. And crimes against health must be treated like crimes against life.How common are counterfeit drugs in developing countries?
The World Health Organization estimates that 1 in 10 medicines in low- and middle-income countries are substandard or falsified. In some regions, like parts of Africa and Southeast Asia, the rate jumps to 30% or higher. For malaria drugs specifically, up to 50% of those sold in border areas are fake.
Can you tell fake medicine from real medicine by looking at it?
It’s extremely hard. Criminals now use 3D printing and high-quality printing to copy packaging with 99% accuracy. Even trained pharmacists can’t spot the difference without lab tools. The only reliable way is through verification systems like SMS codes, blockchain tracking, or chemical testing kits.
What are the most common types of counterfeit drugs?
Antibiotics (35% of cases), antimalarials (25%), heart medications (20%), and painkillers (15%) are the most commonly counterfeited. These are drugs people need urgently, and they’re often expensive-making them prime targets for criminals.
Do fake drugs cause antibiotic resistance?
Yes. When fake antibiotics contain too little active ingredient, they don’t kill all the bacteria. The survivors become resistant. These superbugs then spread, making real antibiotics useless. The WHO calls this one of the biggest global health threats of our time.
Are there any safe ways to buy medicine online in developing countries?
Only if the website is officially linked to the national medicine regulatory authority. In Ghana, Kenya, and Nigeria, governments have partnered with verified online pharmacies. Look for official seals, government domain names (.gov), and verification codes on the packaging. Never buy from social media ads or unknown websites.
What should I do if I suspect I’ve taken a fake drug?
Stop taking it immediately. Contact your local health clinic or pharmacy and report the batch number. If you feel worse-especially after taking antibiotics or malaria drugs-seek medical help right away. Document everything: the packaging, receipt, and symptoms. Reporting fake drugs saves lives.


vinoth kumar
December 2, 2025 AT 16:22Been working with rural clinics in Odisha, and this hits hard. We’ve seen parents bring empty antibiotic packets, thinking the medicine ‘just didn’t work.’ No one knew it was fake. We started training ASHA workers to check pill texture and color-turns out, fake ones are often too smooth, too perfect. Real ones have slight imperfections. It’s not foolproof, but it’s something. We’ve saved at least 12 kids this year just by teaching people to feel the pill.
Also, the mPedigree system? We got it working on basic Androids. Even folks who’ve never used the internet can text a code. It’s not glamorous, but it works.
We need more of this. Not just tech-training. Community trust. And honestly? Less focus on big pharma profits and more on real people dying in villages no one visits.
Gene Linetsky
December 3, 2025 AT 21:14Let’s be real-this whole fake drug thing is just a distraction. The real problem? Western governments and WHO pushing their ‘solutions’ while ignoring the fact that poor countries can’t afford real medicine because Big Pharma prices are gouging. The ‘counterfeit’ drugs? They’re often just cheaper generics made in India or China-stuff the West bans because it doesn’t meet their $1000-per-pill profit model. The kid dies? Maybe. But at least he got something. The system is rigged. The real criminals are the ones charging $12 for a malaria pill that costs 12 cents to make.
And don’t even get me started on blockchain. You think a village in Malawi needs a blockchain ledger? They need food. And $0.20 pills. Not a digital fingerprint.
Ignacio Pacheco
December 4, 2025 AT 02:54Wow. So we’re now treating pharmaceutical fraud like it’s a moral failing of the global south? Interesting. Let’s not forget the 2018 case in Nigeria where a WHO-approved distributor shipped 50,000 fake antimalarials-verified, stamped, and cleared through official channels. The WHO even issued a press release praising the ‘supply chain efficiency.’
And now we’re blaming villagers for buying cheap pills? Meanwhile, the same companies that make these fake drugs are the ones funding the ‘verification tech’ we’re told to trust. Blockchain? Sure. But who owns the nodes? Who audits the auditors?
It’s not a crime of poverty. It’s a crime of corporate negligence. And you’re all just rearranging deck chairs on the Titanic while the real architects sip champagne in Geneva.
Jim Schultz
December 5, 2025 AT 15:16Oh, please. Let’s not pretend this is about ‘justice’ or ‘human rights.’ This is a supply chain failure wrapped in emotional manipulation. You cite 100,000 children? Where’s your peer-reviewed source? The WHO’s 2023 report says 1 in 10 medicines are substandard-that’s 10%. Not 30%. Not 50%. You’re inflating numbers to trigger guilt.
And ‘toxic chemicals’? Name one. Lead? Mercury? Cadmium? You say ‘paint thinner’-but you can’t cite a single confirmed case of paint thinner in a counterfeit antimalarial. Ever. That’s fearmongering. The real killer? Antibiotic resistance from underdosing-which is a medical problem, not a criminal one.
Also, ‘mPedigree’? It’s a startup with 12 employees. You think that’s scalable across 50 countries? Please. You’re romanticizing a Band-Aid. The real solution? Deregulate generic manufacturing. Let India flood the market. Prices drop. Fakes disappear. Simple. But too inconvenient for your ‘global will’ fantasy.
Kidar Saleh
December 5, 2025 AT 23:38I’ve spent the last five years in Ghana and Kenya, and I can tell you this: the most powerful tool isn’t blockchain or solar kits. It’s the village grandmother who remembers what real medicine tastes like. She’s been buying pills for 40 years. She knows the difference between the bitter tang of real artemisinin and the chalky, sweet taste of the fakes.
We trained 800 of these women as ‘pill elders’-no tech, no apps, just lived knowledge. They’ve flagged over 1,200 fake batches. No one in a lab ever noticed them. But she did.
Technology won’t save us. Trust will. And trust is built in the quiet moments-when someone shares a cup of tea and says, ‘This one doesn’t feel right.’
That’s the real verification system. And it’s already working.
Chloe Madison
December 7, 2025 AT 20:29As a former pharmacist in rural Ohio, I’ve seen the same patterns here-people skipping doses because they can’t afford their meds. The U.S. has a $100 insulin crisis. We call it ‘pharmaceutical apartheid.’ The same logic applies globally. People aren’t choosing fake drugs because they’re stupid-they’re choosing them because they’re desperate.
And let’s be honest: if your child is dying of pneumonia and the real antibiotic costs $10, but the fake one costs $1 and you have $1.50 to your name-you’re not a criminal. You’re a parent.
Stop blaming victims. Start fixing the system. Make real drugs affordable. Subsidize them. Tax the profits of Big Pharma. Redirect the billions spent on military aid to medicine access. This isn’t charity. It’s justice. And it’s not that hard to do.
Stop talking about tech. Start talking about economics. And then act.
Vincent Soldja
December 8, 2025 AT 02:44Interesting. But where are the citations for the 100,000 child deaths? The WHO says 1 in 10 medicines are substandard. That’s 10%. Not 100,000 children. Also, counterfeit drugs are not the leading cause of child mortality. Malaria, malnutrition, lack of clean water-those are. This article conflates correlation with causation. The real issue is systemic poverty. Not fake pills.
Makenzie Keely
December 9, 2025 AT 17:40Let’s not sugarcoat this: fake drugs are a humanitarian emergency that’s being ignored because it doesn’t fit neatly into Western media narratives. We don’t see headlines like ‘Child Dies of Fake Antibiotic in Malawi’-we see ‘Celebrity’s New Diet Pill Causes Outrage.’
But here’s what’s happening: every time a child dies from a counterfeit malaria drug, it’s not just a death-it’s a failure of global governance. And we’re letting it happen because it’s ‘over there.’
The mPedigree system? Brilliant. Solar testing kits? Life-changing. But they’re being deployed in 12 countries out of 136 where the problem exists. Why? Because funding goes to flashy tech, not grassroots solutions. And because no one in Brussels or Washington wants to admit that the global supply chain is corrupt.
It’s not about ‘willpower.’ It’s about priorities. And right now, profit beats life. We need to change that. Not tomorrow. Today.
Francine Phillips
December 11, 2025 AT 02:36Yeah, fake drugs are bad. But honestly, I don’t know what to do about it. I feel bad, but I’m just one person. I buy my meds from CVS. I don’t even know how any of this works. I guess I should donate? But I’m broke. So I just scroll past these posts. Sorry. Not sorry. But also, kinda sorry.
Katherine Gianelli
December 12, 2025 AT 15:36I remember sitting with a nurse in Uganda last year. She had a box of 200 fake malaria pills she’d confiscated. She didn’t throw them away. She didn’t burn them. She held one in her hand and said, ‘This one could’ve been my son.’
That’s the heart of this. Not the numbers. Not the blockchain. Not the $50,000 machines.
It’s a mother holding a pill that didn’t save her child. And then choosing to keep fighting anyway.
So if you want to help? Don’t just donate. Go listen. Sit with someone who’s lost someone. Let them tell you their story. Then speak up. Because silence is the real counterfeit here.
Joykrishna Banerjee
December 14, 2025 AT 06:02Let’s not pretend this is a ‘developing world’ problem. The U.S. has 40% of its generic drugs sourced from China. The FDA’s inspection rate? 1.5%. The EU? 2%. Meanwhile, we’re lecturing Ghana on ‘verification systems’? The hypocrisy is staggering. The real counterfeiters are the ones who outsource production to unregulated factories and then slap a ‘Made in USA’ label on it.
And mPedigree? A cute little NGO. But it’s funded by Gates Foundation-so of course it’s ‘sustainable.’ They don’t want to fix the system. They want to control it. Blockchain? It’s just digital colonialism with a QR code.
Stop romanticizing ‘solutions’ that don’t challenge the power structure. The problem isn’t fake pills. It’s capitalism.
Myson Jones
December 14, 2025 AT 07:18Thank you for raising awareness about this critical issue. The global pharmaceutical supply chain is undeniably vulnerable, and the consequences of substandard and falsified medical products are both tragic and preventable. I believe that international collaboration, coupled with robust regulatory frameworks and equitable access to affordable therapeutics, must be prioritized at the highest levels of policy-making. The ethical imperative is clear, and the technological tools already exist to mitigate these risks. What is required now is sustained political will and coordinated multilateral action.
parth pandya
December 15, 2025 AT 23:29in india we have this problem too but its mostly in rural areas where people buy medicine from local shops without prescription. i saw a guy buy fake dolo 650 and he got sick. we told him to go to hospital but he said 'it's cheap, i can't afford real one'. i think the govt should make real medicine cheaper or give free to poor. also pharma companies should be punished more. they are killing people