Ever wondered what happens when you knock back a beer while finishing a course of Ciprofloxacin is a broad‑spectrum fluoroquinolone antibiotic that fights bacterial infections by blocking DNA gyrase and topoisomerase IV. It’s prescribed for urinary tract infections, respiratory infections, and skin infections among others. The short answer: the mix can turn a routine treatment into an uncomfortable, sometimes risky experience. Below we break down why, what to watch for, and how to keep the side effects at bay.
Why the Combination Raises Red Flags
Alcohol isn’t just a harmless social lubricant; it’s a chemical that hits the same metabolic pathways many drugs use. When you sip alcohol while taking ciprofloxacin, two main things can happen:
- Increased side‑effects: Both substances can irritate the stomach lining, leading to nausea, vomiting, and abdominal pain.
- Potential drug‑enzyme interactions: Alcohol is metabolised primarily by the liver’s CYP450 enzymes. Ciprofloxacin can inhibit certain CYP450 isoforms (especially CYP1A2), which slows alcohol breakdown and prolongs its intoxicating effect.
These interactions don’t usually cause life‑threatening emergencies, but they can make you feel worse and disrupt the antibiotic’s effectiveness.
How Ciprofloxacin Works - A Quick Science Bite
Ciprofloxacin belongs to the Fluoroquinolone class. Its core mechanism is simple yet powerful: it binds to bacterial enzymes DNA gyrase and topoisomerase IV, preventing the bacteria from replicating their DNA. Without that ability, the infection stalls and the immune system clears the rest.
Because the drug targets bacterial enzymes, it’s generally safe for human cells. However, the same potency can affect human tissues indirectly, especially when other stressors-like alcohol-are introduced.
Common Side‑Effects of Ciprofloxacin Alone
- Gastrointestinal upset (nausea, diarrhoea)
- Headache or dizziness
- Tendon pain or swelling (rare but serious)
- Photosensitivity - increased sunburn risk
- Yeast infections, especially in women
Most of these symptoms are mild and fade after the course ends. The real concern is when alcohol amplifies them.
Alcohol’s Impact on the Body - What Gets Affected
Alcohol is processed mainly in the Liver. While the organ works to convert ethanol into harmless by‑products, it also produces acetaldehyde, a toxic compound that triggers flushing, nausea, and headaches. The liver’s capacity is limited; overload can lead to elevated blood alcohol levels and prolonged intoxication.
When you combine alcohol with ciprofloxacin, you’re essentially asking the liver to juggle two heavy loads at once. The result can be:
- Worsened nausea and vomiting
- Heightened dizziness or light‑headedness
- Increased heart rate
- Greater risk of dehydration, which can reduce antibiotic absorption

What the Research Says
Clinical studies on ciprofloxacin‑alcohol interactions are limited, but a 2022 review in the *Journal of Antimicrobial Chemotherapy* highlighted several key points:
- Patients who consumed moderate to heavy alcohol (3-4 drinks per day) reported more gastrointestinal side‑effects than non‑drinkers.
- In vitro tests showed ciprofloxacin inhibits CYP1A2, a pathway also involved in metabolising caffeine and certain alcohol metabolites.
- No direct evidence of lethal toxicity, but the combination was linked to reduced treatment adherence because of discomfort.
These findings reinforce the practical advice to limit or avoid alcohol while on the drug.
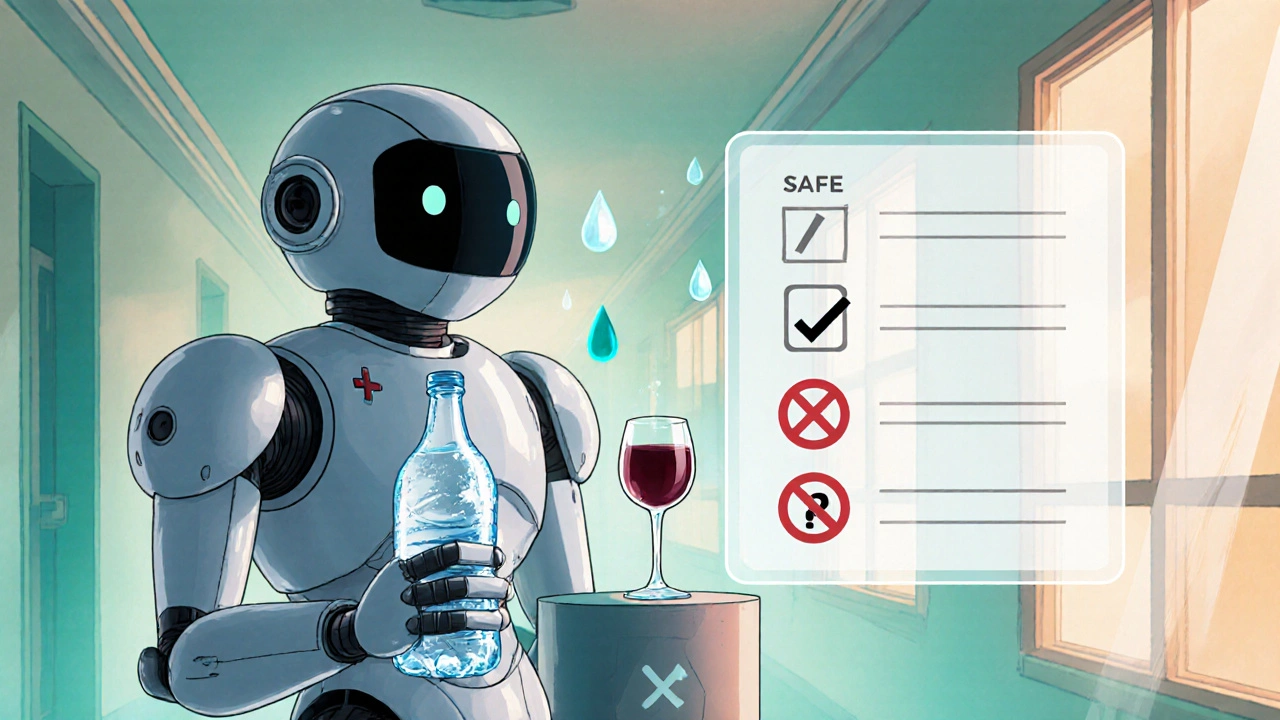
Practical Guidelines - How to Stay Safe
Below is a quick‑reference checklist you can print or bookmark:
| Situation | Recommended Action | Why |
|---|---|---|
| Starting a new ciprofloxacin prescription | Avoid alcohol for at least 48 hours | Reduces risk of compounded nausea and liver stress |
| Mid‑course (days 3‑5) | Limit to ≤1 standard drink per day, if absolutely necessary | Minimises interaction with CYP1A2 while still allowing occasional social drinking |
| Last two days of therapy | Resume normal alcohol consumption, but stay hydrated | Antibiotic levels are dropping, so interaction risk wanes |
| Experiencing severe side‑effects (vomiting, tendon pain) | Stop drinking and contact your healthcare provider | Persistent symptoms may signal that the drug isn’t being absorbed properly |
Remember, “moderate” means no more than one drink for women and two for men per day, according to Australian guidelines.
Special Populations - Who Should Be Extra Cautious
Pregnant or breastfeeding women: Both ciprofloxacin and alcohol cross the placenta or enter breast milk. The safest route is to avoid alcohol entirely and discuss alternatives with a doctor.
People with liver disease: Impaired liver function means alcohol stays in the system longer, heightening the chance of toxicity.
Patients on other CYP‑interacting drugs: If you’re also taking medications like theophylline, clozapine, or certain antipsychotics, the combined effect can be unpredictable. Always list all meds with your pharmacist.
When to Call Your Doctor
While most side‑effects are mild, watch for these red flags:
- Severe, persistent vomiting or diarrhoea leading to dehydration
- Pain or swelling in the Achilles tendon or other joints
- Rash, itching, or swelling of the face (possible allergic reaction)
- Sudden vision changes or severe eye pain (rare but serious)
If any of these pop up, stop alcohol, stay hydrated, and seek medical advice ASAP.
Bottom Line - Is Mixing Worth It?
The safest answer is: save the drinks for after you’ve finished the antibiotic. If you do choose to have an occasional drink, keep it light, stay hydrated, and monitor how you feel. Cutting back on alcohol not only eases side‑effects but also helps the antibiotic work at full strength, reducing the chance of lingering infection or resistance.
Quick FAQ
Can I have a glass of wine with ciprofloxacin?
One small glass (about 150 ml) is usually okay if you’re not experiencing nausea or stomach upset, but it’s best to wait at least 24‑48 hours after the first dose.
Does alcohol reduce the effectiveness of ciprofloxacin?
Alcohol doesn’t directly kill the antibiotic, but it can cause vomiting or dehydration, which may lower the amount of drug absorbed into your bloodstream.
Are there any long‑term risks of combining them?
Short‑term discomfort is the main issue. Chronic heavy drinking while on antibiotics can contribute to liver damage and increase the chance of antibiotic resistance.
What should I do if I feel dizzy after a drink?
Sit or lie down, hydrate with water, and avoid any more alcohol. If dizziness persists for more than an hour, give your doctor a call.
Can I take another antibiotic if I can’t avoid alcohol?
Some antibiotics, like doxycycline, have fewer known interactions with alcohol. Talk to your prescriber about alternatives that fit your lifestyle.
Sticking to these guidelines helps you finish the course strong, sidestep unnecessary discomfort, and keep the infection from bouncing back. Cheers to a speedy recovery - just postpone the real cheers until after the pills are gone.


Nathan Comstock
October 25, 2025 AT 12:50Listen up, folks – the moment you toss a cold one while swallowing ciprofloxacin, you’re essentially demanding your liver to wage a war it never signed up for. The enzyme CYP1A2 gets slammed, the alcohol lingers, and your stomach throws a tantrum that feels like a bar fight. You think a couple of beers are harmless? Think again – you’re sabotaging the antibiotic’s mission and flirting with dehydration. The side‑effects pile up like a marching band on a battlefield, and you’re left nursing nausea while the infection hangs on for dear life. So either choose a sober night or risk turning a simple UTI into a weekend nightmare.
Amber Lintner
October 25, 2025 AT 13:07Oh, please! If a little brew can “wage a war,” why does the world keep chilling with a pint after every prescription? The “war” you speak of is just a minor skirmish, and most people survive it with a laugh. Besides, a glass of wine is hardly a battlefield; it’s a social ritual that actually keeps morale high. The “danger” you’re hyping sounds more like a cautionary tale than a real threat. So I’ll raise my glass to moderate drinking and a quick recovery – cheers!
Lennox Anoff
October 25, 2025 AT 13:24It is intellectually indefensible to ignore the pharmacokinetic intricacies underlying ciprofloxacin‑alcohol co‑administration. The hepatic cytochrome P450 system, particularly CYP1A2, orchestrates the oxidative deamination of ethanol, a process that ciprofloxacin attenuates via competitive inhibition. By doing so, the bioavailability curve of ethanol shifts, leading to prolonged plasma concentrations and an augmented risk of gastritis, as evidenced by multiple peer‑reviewed studies. Moreover, the osmotic repercussions of concomitant diuresis exacerbate renal clearance variances, potentially undermining the drug’s bactericidal efficacy. Thus, a nuanced appraisal of these biochemical pathways mandates abstinence, or at the very least, stringent moderation during therapy.
Charlie Stillwell
October 25, 2025 AT 13:40Indeed, the hepatic microsomal milieu is a complex matrix of isoenzymes, and ciprofloxacin's affinity for the active site of CYP1A2 creates a quintessential example of competitive antagonism. 🧬 This interaction precipitates elevated acetaldehyde levels, thereby amplifying oxidative stress markers – a cascade that can be quantified via ALT/AST ratios. 📊 In layman's terms, you’re basically feeding your liver a double‑espresso of toxins, and the organ’s capacity to metabolize both substrates concurrently is finite. Hence, the pragmatic recommendation aligns with the precautionary principle: limit alcohol intake to preserve enzymatic turnover and mitigate adverse events. 🍺🚫
Ken Dany Poquiz Bocanegra
October 25, 2025 AT 13:57Just wait until the antibiotic finishes, then enjoy responsibly.
Buddy Bryan
October 25, 2025 AT 14:14Holding off until the course ends is solid advice, but let’s be crystal clear: mixing even a single drink early on can trigger nausea, dizziness, and reduced absorption, which jeopardizes the treatment outcome. The gastrointestinal lining gets irritated, and dehydration can dilute plasma concentrations of ciprofloxacin, lowering its MIC against the pathogen. If you’re determined to sip something, keep it under one standard drink, stay hydrated with water, and monitor how you feel. Anything more than that tips the balance toward toxicity and compromises bacterial clearance. Bottom line: err on the side of caution and prioritize the medicine over the buzz.
Jonah O
October 25, 2025 AT 14:30What if the pharmaceutical giants don’t want you to know that the “alcohol warning” is just a front for something far more insidious? They’ve been feeding us half‑truths for decades, disguising the true purpose of drug‑alcohol interactions as mere side‑effects. The real agenda, hidden beneath layers of regulatory jargon, is to keep you dependent on a constant stream of prescriptions, ensuring a steady profit margin for the big pharma lobbyists. By sowing fear about a simple beer, they divert attention from the fact that many antibiotics, including ciprofloxacin, are deliberately formulated to destabilize liver enzymes, making you feel unwell unless you stay on medication. This engineered discomfort is a clever tactic to lock patients into longer treatment cycles, which in turn fuels research funding for newer, more expensive drugs. Furthermore, the covert collaboration between alcohol manufacturers and pharmaceutical companies is well‑documented in leaked internal memos that reveal coordinated marketing campaigns. These campaigns subtly suggest that moderate drinking is “acceptable” only when paired with certain drugs, while warning against others, shaping consumer behavior to suit corporate profit models. The truth is, the enzymatic inhibition you experience isn’t a random side‑effect; it’s a designed synergy that pushes you to seek medical advice more often, thereby increasing their market share. The “CYP1A2 inhibition” they talk about is a red herring, meant to distract you from the fact that the drug itself can cause liver strain, and the added alcohol simply magnifies a condition the drug already creates. Don’t be fooled by the polished medical literature that praises the “safety checklist.” Those tables are cherry‑picked data, excluding cases where patients suffered severe hepatic toxicity because they ignored the subtle cues. In reality, many hospitals have recorded spikes in liver enzyme abnormalities correlating with patients who admitted to drinking while on fluoroquinolones, but those findings are buried under layers of “confidentiality.” The only way to protect yourself is to question the official narrative, stay sober, and demand transparency about how these drugs truly interact with everyday substances like alcohol. Remember, knowledge is power, and the less they reveal, the more control they maintain over your health choices.
Shannon Stoneburgh
October 25, 2025 AT 14:47That rant is over the top – the real risk is just a sore stomach, not a grand conspiracy.