Chronic kidney disease doesn’t announce itself. It creeps in silently.
By the time most people feel symptoms-fatigue, swelling, trouble sleeping-it’s often too late to stop the damage. One in seven American adults has chronic kidney disease (CKD), and up to 90% don’t know it. That’s not because they’re ignoring their health. It’s because the early signs are invisible. No pain. No fever. No red flags on a routine checkup-unless your doctor orders the right tests.
CKD isn’t just about aging kidneys. It’s the quiet result of uncontrolled diabetes, high blood pressure, or genetics. Left unchecked, it can lead to kidney failure, dialysis, or transplant. But here’s the truth: if you catch it in stage 1 or 2, you have a strong shot at stopping it cold. Not just slowing it-stopping it. And that starts with two simple blood and urine tests.
What exactly is chronic kidney disease?
CKD isn’t one disease. It’s a label for long-term damage to your kidneys that lasts three months or more. Your kidneys don’t just filter waste. They balance fluids, regulate blood pressure, make red blood cells, and activate vitamin D. When they’re damaged, all of that starts to break down.
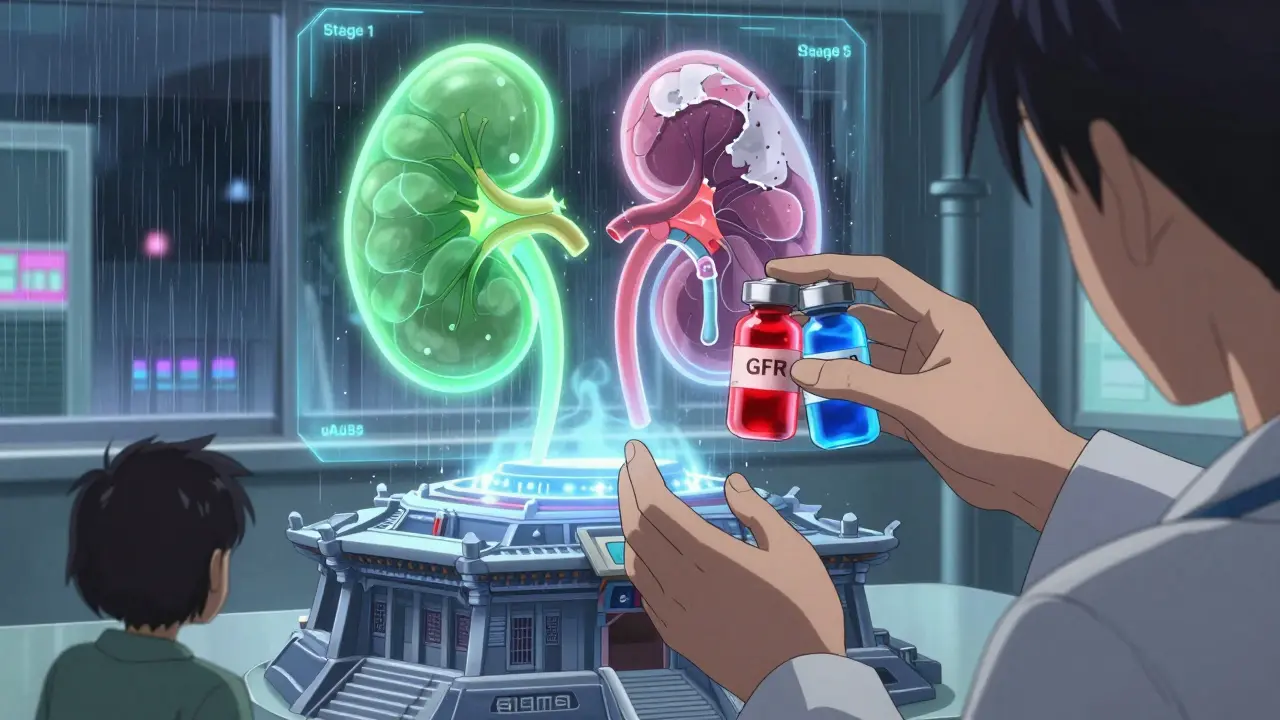
The medical definition is clear: either your estimated glomerular filtration rate (eGFR) is below 60 for three months, or you have signs of kidney damage-like protein in your urine-even if your eGFR is normal. That second part is critical. Many people assume normal creatinine means healthy kidneys. It doesn’t. Creatinine levels can look fine even when your kidneys are leaking protein. That’s why you need both tests.
Stage 1 CKD means your eGFR is normal (90 or higher) but you have protein in your urine. Stage 2 means your eGFR is slightly lowered (60-89) with ongoing damage. These are the stages where you can still turn things around. By stage 3, you’ve lost 40-50% of kidney function. By stage 5, you’re facing dialysis.
The two tests that save lives
Doctors used to rely on serum creatinine alone. That’s like checking your car’s oil light without looking at the engine. You might miss the leak until it’s too late.
Today, guidelines from KDIGO and the National Kidney Foundation demand two tests:
- eGFR: Calculated from your blood creatinine, age, sex, and race. It estimates how well your kidneys filter waste. The CKD-EPI equation is the current gold standard.
- uACR: Urine albumin-to-creatinine ratio. This measures how much protein (albumin) is leaking into your urine. A result of 30 mg/g or higher means damage is happening.
You need both. One alone isn’t enough. A 2018 study found that using only creatinine missed 30-40% of early CKD cases. That’s tens of millions of people walking around thinking they’re fine.
Some people need more. If your eGFR is borderline (45-59) and you don’t have diabetes or high blood pressure, your doctor might check cystatin C-a different blood marker that’s less affected by muscle mass or diet. Or they might order an ultrasound to look for structural issues. But for most people, eGFR and uACR are all you need to start.
Who should be tested-and how often?
Not everyone needs yearly screening. But if you fit any of these categories, you’re at risk and should be tested annually:
- Diabetes: Type 2? Get tested at diagnosis. Type 1? Start testing five years after diagnosis. This is non-negotiable. The American Diabetes Association requires it.
- High blood pressure: Especially if it’s been hard to control. Every visit should include a check of your kidney function.
- Family history: If a close relative had kidney failure, your risk jumps.
- Age over 60: Kidney function naturally declines, but that doesn’t mean damage is normal.
- Black, Native American, or Hispanic heritage: These groups have 2-4 times higher risk due to genetic, social, and healthcare access factors.
- Chronic use of NSAIDs: Ibuprofen, naproxen, and similar drugs can harm kidneys over time.
Don’t wait for symptoms. By then, it’s too late. If you’re in one of these groups, ask your doctor for eGFR and uACR at your next visit. If they say, “We only check creatinine,” push back. That’s outdated practice.
What happens if you catch it early?
Here’s the hopeful part: early detection isn’t just about monitoring. It’s about reversing damage.
Studies show that with the right steps, you can cut your annual eGFR decline from 3.5 mL/min to just 1.2 mL/min. That’s the difference between reaching kidney failure in 10 years versus never getting there.
Three proven interventions work best:
- Medications: SGLT2 inhibitors (like empagliflozin or dapagliflozin) were originally for diabetes. Now we know they protect kidneys-even in non-diabetics. The CREDENCE trial showed a 32% drop in kidney failure risk when started in stage 2 CKD with proteinuria.
- Blood pressure control: Target under 130/80. The SPRINT trial showed this cuts progression risk by 27% compared to the old target of 140/90.
- Diet and lifestyle: Reduce salt. Avoid processed foods. Maintain a healthy weight. Quit smoking. These aren’t “nice to haves.” They’re medical necessities.
Some people think, “I don’t have diabetes, so I’m safe.” Wrong. High blood pressure alone causes nearly half of all CKD cases. And obesity? It’s the fastest-growing risk factor.

Why aren’t more people being tested?
There’s a gap between what guidelines say and what happens in clinics.
A 2022 study found only 53% of primary care doctors order both tests for at-risk patients. In rural areas, it’s as low as 32%. Why? Electronic health records don’t prompt for both. Doctors forget. Patients don’t ask. And insurance doesn’t always cover it unless there’s a clear diagnosis.
One patient on Reddit shared: “My doctor checked creatinine for 10 years. When they finally did uACR, I was stage 3.” That’s not rare. That’s the norm.
Meanwhile, clinics that use “CKD dashboards”-automated alerts in patient records-see screening rates jump by 60%. The Kidney Precision Medicine Project created standardized reporting templates that cut diagnostic errors by 35%. Simple tools, big results.
And here’s the kicker: Medicare Advantage plans are now tying provider payments to early CKD detection. Humana saw a 19% increase in early-stage diagnoses after requiring dual testing. That’s not charity. That’s economics. Preventing one case of kidney failure saves $120,000 over five years.
The future is here-so why wait?
In May 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that analyzes 32 data points to predict who’s at risk of CKD before their eGFR drops. It’s not in every doctor’s office yet, but it’s coming.
Also in 2023, the Biden administration launched a $150 million push to implement dual testing in federally funded clinics by 2026. That could identify over a million undiagnosed cases.
And the big debate? Race-adjusted eGFR formulas. For years, labs automatically adjusted creatinine results upward for Black patients, assuming they had more muscle mass. That meant many Black patients were told their kidneys were “fine” when they weren’t. Removing race from the formula could increase early detection in Black populations by over 12%.
It’s not about blame. It’s about accuracy. And accuracy saves lives.
What you can do right now
You don’t need a specialist. You don’t need a referral. You just need to ask.
If you’re at risk, say this at your next appointment:
“I’d like my eGFR and uACR tested. I’ve heard that’s the only way to catch kidney damage early.”
If your doctor says, “We only check creatinine,” say: “I understand that’s what you’ve done before, but current guidelines require both tests. Can you order them?”
Bring a printed copy of the National Kidney Foundation’s CKD screening guidelines if needed. Most doctors will comply.
And if you’ve already been diagnosed with early CKD? Don’t panic. You’re not alone. You’re not doomed. You’re in the window where action matters most. Stick with your meds. Watch your salt. Control your blood pressure. Get your labs done every 6-12 months. You can still live a full, active life.
Chronic kidney disease doesn’t have to be a death sentence. It just has to be found.
Can you have chronic kidney disease with normal creatinine?
Yes. Creatinine alone is not enough. You can have normal creatinine but still have protein in your urine (uACR ≥30 mg/g), which is the earliest sign of kidney damage. This is why both eGFR and uACR are required for diagnosis. Many people are misdiagnosed as healthy because their doctors only check creatinine.
How often should I get tested for CKD?
If you have diabetes, high blood pressure, a family history of kidney failure, or are over 60, get tested every year. If you’re at high risk due to race or chronic NSAID use, annual testing is also recommended. If you’ve already been diagnosed with early-stage CKD, your doctor may want labs every 6 months to track progress.
Does CKD always lead to dialysis?
No. In fact, most people with early-stage CKD never reach dialysis. With proper management-medications like SGLT2 inhibitors, blood pressure control, diet changes, and regular monitoring-progression can be stopped or slowed dramatically. Up to 70% of stage 1 and 2 patients avoid kidney failure if they act early.
Can lifestyle changes really reverse kidney damage?
You can’t undo scarring, but you can stop further damage-and even improve function. Losing weight, cutting salt, quitting smoking, and controlling blood pressure and blood sugar reduce stress on the kidneys. Studies show this can slow eGFR decline by more than 65%. In some cases, protein in the urine drops significantly, which is a strong sign of recovery.
Are over-the-counter painkillers dangerous for kidneys?
Yes. Regular use of NSAIDs like ibuprofen, naproxen, or aspirin can damage kidneys over time, especially if you already have high blood pressure, diabetes, or are over 60. Occasional use is usually fine, but if you’re taking them daily for headaches or arthritis, talk to your doctor about alternatives. Kidney damage from NSAIDs is often reversible if caught early.
What’s the difference between stage 3a and 3b CKD?
Stage 3a means your eGFR is 45-59-mild to moderate loss. Stage 3b is 30-44-moderate to severe loss. Both mean you’ve lost 30-50% of kidney function. The key difference is urgency: stage 3b patients need more frequent monitoring, stricter blood pressure control, and often referral to a nephrologist. Stage 3a can still be managed in primary care if caught early and treated aggressively.

Sheila Garfield
January 31, 2026 AT 14:27Also, NSAIDs are a silent killer. I used ibuprofen daily for years. Never connected it to my fatigue.
Shawn Peck
February 2, 2026 AT 09:09Niamh Trihy
February 2, 2026 AT 20:45Yanaton Whittaker
February 3, 2026 AT 18:27Diana Dougan
February 4, 2026 AT 05:13Bobbi Van Riet
February 5, 2026 AT 16:57Holly Robin
February 6, 2026 AT 09:19Lily Steele
February 7, 2026 AT 05:25Amy Insalaco
February 7, 2026 AT 10:55