Boxed Warning Timeline Calculator
Calculate Boxed Warning Timeline
Boxed warnings (black box warnings) are the FDA's strongest safety alert for prescription drugs. This tool estimates how long it typically takes for these warnings to appear for different drug classes based on FDA data.
Timeline Results
Key Statistics
- Median Time 11 years
- Warning Prevalence 40%
- Most Common Update Type Minor Updates
Drug Class Details
Select a drug class to view specific details
Boxed Warning Timeline Visualization
The timeline shows the typical progression of boxed warnings for prescription drugs. Most warnings appear within the first decade of a drug's approval, but rare side effects may take years to identify.
When a drug comes with a boxed warning, it’s not just a footnote-it’s a red flag. This isn’t a generic caution. It’s the FDA’s strongest safety alert, printed in bold black letters inside a thick black border at the very top of a prescription drug’s prescribing information. If you’re a doctor, pharmacist, or someone managing long-term medication, you need to know how these warnings change-and why it matters.
What Exactly Is a Boxed Warning?
A boxed warning, sometimes called a black box warning (BBW), is the FDA’s most serious safety notice for prescription drugs. It doesn’t talk about mild side effects like headaches or nausea. It’s reserved for risks that can cause serious injury, disability, or death. Think: sudden heart failure, suicidal behavior, liver failure, or life-threatening infections. These warnings were first introduced in 1979. The format hasn’t changed much since: a bold header in ALL CAPS, bullet points listing the specific dangers, and a thick black border that makes it impossible to miss. The FDA requires this format under 21 CFR 201.57(e). It’s placed right at the start of the Prescribing Information section-before even the contraindications. That’s intentional. The FDA wants you to see this before you even read the rest. As of 2024, about 40% of all prescription drugs in the U.S. carry at least one boxed warning. That’s over 600 medications. The most affected classes? Antipsychotics (87% have one), anticoagulants (78%), and diabetes drugs (63%). These aren’t rare treatments-they’re widely used. So if you’re prescribing or taking any of these, you’re likely dealing with a boxed warning.Why Do Boxed Warnings Change?
Boxed warnings aren’t written in stone. They evolve as more data comes in after a drug hits the market. That’s because many serious side effects only show up after thousands of people use the drug for months or years. Clinical trials, which involve a few thousand patients over a few months, often miss these delayed or rare risks. The FDA tracks every change through its Drug Safety-related Labeling Changes (SrLC) database, which launched in January 2016. Before that, changes were scattered across old MedWatch reports and Drugs@FDA. Now, everything is centralized. Since 2016, the database has recorded over 1,800 labeling updates-including 147 new boxed warnings. Changes fall into three categories:- New warnings (29%): The drug gets a boxed warning for the first time. Example: Aduhelm’s 2023 warning about brain swelling and bleeding (ARIA) after post-marketing data showed it was more common than expected.
- Major updates (32%): The warning gets expanded. Example: Fluoroquinolone antibiotics (like Cipro) had their warning updated in 2022 to include persistent, disabling side effects like tendon ruptures and nerve damage that can last years.
- Minor updates (40%): Clarifications, wording tweaks, or added monitoring recommendations. Example: Adding a note that patients on certain antipsychotics need baseline EKGs before starting.
How Long Does It Take for a Warning to Appear?
Here’s the uncomfortable truth: it takes a long time. In the 1980s and 1990s, the median time from drug approval to a boxed warning was about 7 years. Today, it’s 11 years. That’s over a decade of patients being exposed to a risk before the FDA acts. Why the delay? It’s not laziness. It’s science. To prove a drug causes a rare but deadly side effect, you need enough cases to rule out coincidence. That takes time. But critics argue the system is too slow. One 2010 study found 71% of serious drug risks were identified more than five years after approval. By then, tens of thousands of people may have been harmed. The FDA’s Sentinel Initiative, launched in 2008, uses real-world data from millions of electronic health records to spot signals faster. It’s cut detection time by about 2.3 years. But even that’s not enough. The FDA is now partnering with OHDSI, a global health data network, to reduce that 11-year gap to under five years by 2027.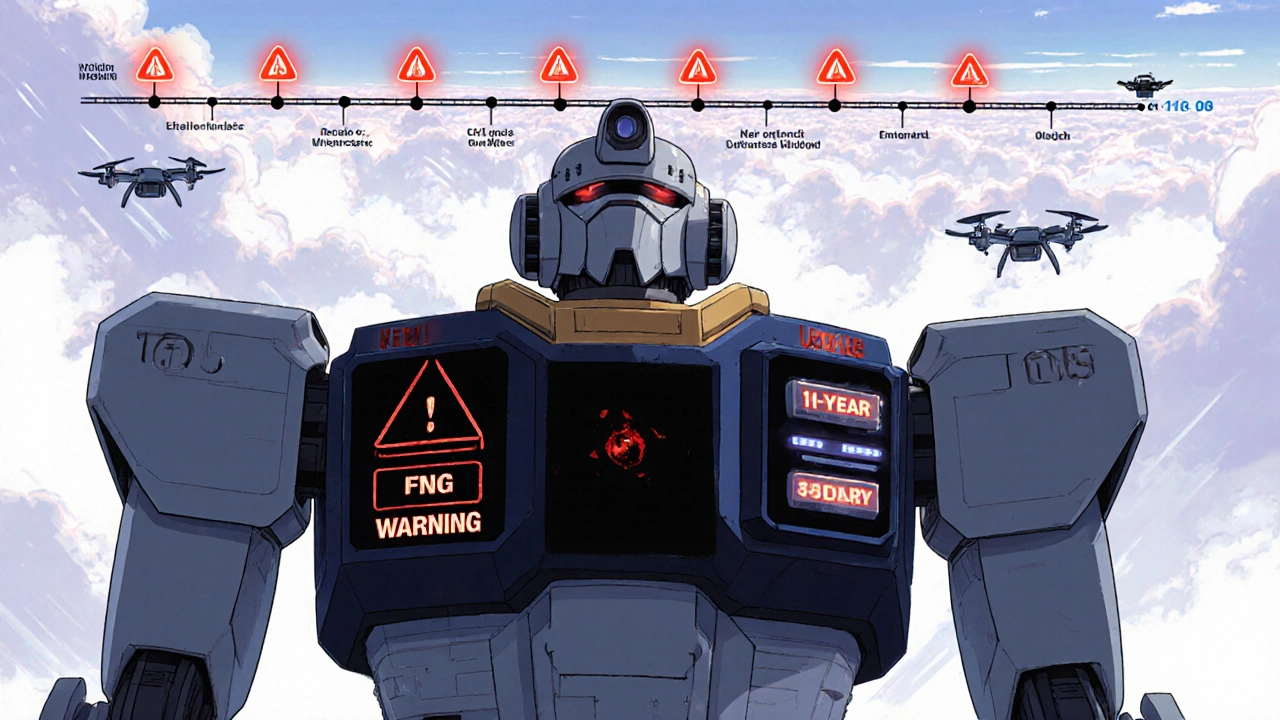
Who Notices These Changes?
Surprisingly, not everyone. A 2017 FDA survey of 500 healthcare providers found that 87% check for boxed warnings when prescribing a new drug. But 63% admitted they sometimes miss updates to existing ones. Why? Because tracking changes is messy. Pharmacists at academic hospitals spend 12 hours a month just reviewing labeling updates. Community pharmacies? Only 38% have formal monitoring systems. Most rely on automated alerts from their pharmacy software-but 41% say those systems flood them with false alarms, so they start ignoring them. Doctors aren’t immune. A 2023 Medscape poll found 52% of physicians believe some boxed warnings are overly cautious. They point to Avandia (rosiglitazone), which got a boxed warning for heart risk in 2007. Many endocrinologists felt it unfairly scared off patients from a drug that helped those who couldn’t use other diabetes meds. The warning stayed even after later studies questioned the risk level.What Happens When a Warning Is Added or Removed?
Changes don’t just sit on a label-they change behavior. After the fluoroquinolone tendon rupture warning was added in 2008, 68% of doctors on Sermo said they changed how they prescribed these antibiotics. Internists cut use the most. The Chantix (varenicline) warning for suicidal thoughts, added in 2009, caused prescriptions to drop by 40% in some clinics. When the FDA removed it in 2016 after new data showed the risk was lower than feared, prescriptions bounced back. But removals are rare. Most warnings stick around-even if the science evolves. That’s because the FDA doesn’t remove warnings lightly. They’re designed to be conservative. It’s easier to add a warning than take one away.What’s Next for Boxed Warnings?
The FDA says the current system is “essential but outdated.” In 2023, they announced a plan to modernize the format by 2026. Pilot tests are already underway. New designs might include:- Color-coded severity levels (red for life-threatening, yellow for serious)
- Icons for monitoring requirements (e.g., a heart icon for EKG checks)
- Links to digital tools like patient risk calculators
What Should You Do?
If you’re a patient:- Ask your doctor: “Does this drug have a boxed warning? Has it changed since I started taking it?”
- Request a Medication Guide. Studies show patient understanding of risks jumps from 42% to 78% when these are provided.
- Don’t stop a drug just because of a warning. Talk to your provider. Many boxed warnings apply only to specific groups-like people with kidney disease or a history of depression.
- Set up a monthly review of the FDA’s SrLC database. Use filters for “BOXED WARNING” and “Updated” to cut through noise.
- Use automated alerts-but don’t rely on them alone. Cross-check with the FDA’s official site.
- Document why you chose to prescribe a drug with a boxed warning. That protects you and helps your patient.
Final Thought: A Warning Is Not a Ban
A boxed warning doesn’t mean a drug is unsafe. It means the risk is real-and you need to know how to manage it. Many drugs with boxed warnings are still vital. They save lives. But they demand attention. The system isn’t perfect. It’s slow. It’s noisy. But it’s the best tool we have to catch dangers that clinical trials can’t see. Tracking changes isn’t optional. It’s part of safe prescribing-and safe taking.What does a boxed warning mean for patients?
A boxed warning means the drug carries a serious, potentially life-threatening risk. It doesn’t mean you can’t take it-it means you and your doctor need to understand the risk, monitor for it, and weigh it against the benefits. Always ask: What are the signs I should watch for? What tests do I need? Is there a safer alternative?
Can a boxed warning be removed?
Yes, but it’s rare. The FDA removes a boxed warning only when new, high-quality evidence shows the risk is much lower than originally thought-or not real. The Chantix psychiatric risk warning was removed in 2016 after follow-up studies showed the link was weaker than first believed. Removal requires strong data and is done cautiously to avoid sending the wrong message.
How often are boxed warnings updated?
The FDA issues about 10-20 new boxed warnings each year, with many more updates to existing ones. Since 2016, over 147 new boxed warnings have been added, and hundreds of updates have been made. Changes happen as soon as the FDA has enough evidence to justify them-usually within 180 days of a safety decision.
Where can I find official updates to boxed warnings?
The FDA’s Drug Safety-related Labeling Changes (SrLC) database is the official source for all changes since January 2016. You can search by drug name, active ingredient, or warning type. For older changes, check the MedWatch archives. Always verify updates on FDA.gov-not third-party sites.
Do other countries have boxed warnings?
The U.S. is the only country with the formal black box format. The European Medicines Agency uses a “black triangle” symbol (▼) to flag new drugs under extra monitoring, but it doesn’t have the same structure or legal weight as a U.S. boxed warning. Other countries rely on different formats, but none match the visibility or regulatory force of the FDA’s system.


Matthew Stanford
November 30, 2025 AT 06:39Boxed warnings are the FDA’s way of saying ‘this could kill you, but we’re not banning it.’ Kinda wild when you think about it.
Olivia Currie
November 30, 2025 AT 08:10OMG I just realized my mom’s been on an antipsychotic with a black box for 8 years and no one ever explained what it actually meant. I’m gonna scream at her pharmacist tomorrow. 😭
Curtis Ryan
December 1, 2025 AT 04:13so like… if a drug has a boxed warning, does that mean its basically a death sentence? i mean i get it, but like… why do we even keep these drugs on the market? also i think the fda is just scared to admit they messed up. 🤷♂️
Rajiv Vyas
December 1, 2025 AT 04:33Let’s be real - the FDA doesn’t care about you. They’re just protecting Big Pharma. The ‘11-year delay’? That’s because they’re waiting for the drug company to pay off the regulators. You think they’d wait that long if it was a Chinese drug? Nope. They’d ban it tomorrow.
farhiya jama
December 2, 2025 AT 01:26Why am I even reading this? I just take my pills and hope for the best. My doctor’s busy. My pharmacist’s on break. My insurance won’t cover the ‘safer’ option. So yeah. I’m just gonna keep swallowing the black box.
Astro Service
December 2, 2025 AT 11:31Black box? More like a red flag for weak Americans. Back in my day, we took meds without a warning label and we liked it. This whole ‘risk management’ crap is just coddling people. If you can’t handle a little heart failure, don’t take the pill. Simple.
DENIS GOLD
December 3, 2025 AT 03:56So the FDA takes 11 years to warn us about a drug that kills people… but they approved TikTok in 11 days? 🤔 Yeah, I see the priorities now.
Ifeoma Ezeokoli
December 4, 2025 AT 05:40I’m from Nigeria and we don’t even have this system. People just get meds from the market and pray. But honestly? I think the US system is too bureaucratic. Maybe we need something between ‘no warning’ and ‘black box.’ Like… a yellow triangle with a gentle reminder? 🤔
Daniel Rod
December 5, 2025 AT 09:56It’s funny how we treat drugs like they’re magic bullets. We want them to fix everything… but we’re terrified of the cost. A boxed warning isn’t a death sentence - it’s a mirror. It shows us how much we rely on chemistry to solve human problems. We need better systems, yes… but also better conversations. ❤️
gina rodriguez
December 5, 2025 AT 20:05My clinic just started using an AI tool that flags boxed warning updates in real time - game changer. I used to miss 3-4 updates a month. Now I catch them all. Small change, big difference. 🙌
Sue Barnes
December 5, 2025 AT 22:08If you’re not checking the SrLC database monthly, you’re not a real clinician. Seriously. This isn’t optional. If you’re still relying on pharmacy alerts, you’re one bad reaction away from a lawsuit. Wake up.