Every year, thousands of older adults end up in the hospital because of a medication that shouldn’t have been prescribed in the first place. It’s not always a mistake-it’s often a routine one. A drug that worked fine at 55 doesn’t always work the same at 75. The body changes. The kidneys slow down. The liver processes less. What was once safe can become dangerous. That’s where the Beers Criteria come in.
What Are the Beers Criteria?
The Beers Criteria are a list of medications that doctors and pharmacists should avoid prescribing to adults aged 65 and older. Developed in 1991 by Dr. Mark Beers and updated every few years since, the latest version came out in 2023 from the American Geriatrics Society (AGS). This isn’t just a suggestion-it’s the most widely used tool in the U.S. to reduce harmful drug use in older people.It’s not about banning drugs. It’s about recognizing that some medications carry more risk than benefit for seniors. For example, a drug that helps with sleep in a 40-year-old might cause confusion, falls, or even delirium in someone over 70. The Beers Criteria highlight those exact risks.
The 2023 update includes 131 specific medication warnings. These are broken into five groups:
- Drugs to avoid in almost all older adults
- Drugs to avoid if you have certain conditions (like dementia, kidney disease, or heart failure)
- Drugs to use with caution
- Drugs that are risky when kidney function is reduced
- Drug combinations that can cause dangerous interactions
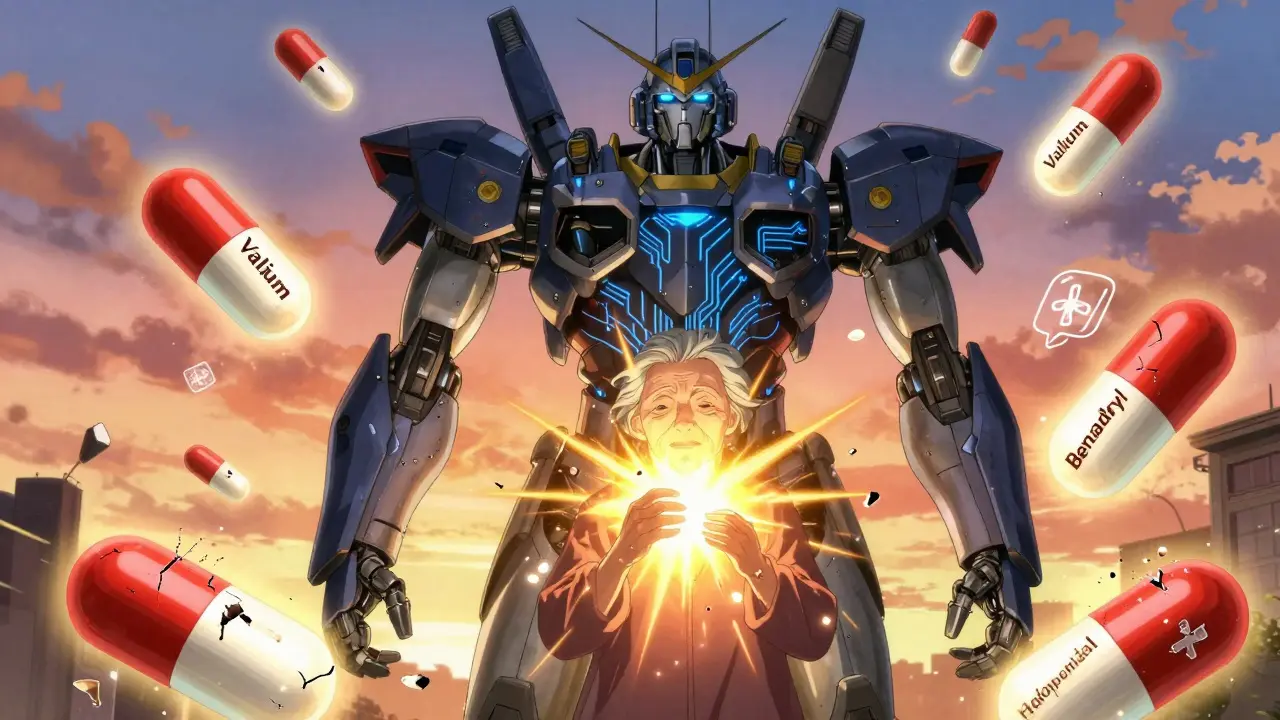
Some of the most common offenders? Benzodiazepines like diazepam (Valium), antipsychotics like haloperidol, and certain antihistamines like diphenhydramine (Benadryl). These are still prescribed regularly-even though they’re linked to memory loss, falls, and increased death risk in older adults.
Why Do These Drugs Still Get Prescribed?
You’d think doctors would know better. But here’s the reality: prescribing for older adults is messy.Many seniors take five, ten, or even fifteen different medications. That’s called polypharmacy. It’s common. It’s often necessary. But it’s also where mistakes happen. A primary care doctor might prescribe a sleep aid because the patient says they can’t sleep. A specialist adds a painkiller. A cardiologist adds a blood thinner. No one’s looking at the full picture.
Time is short. Electronic health records don’t always flag risky combinations. And sometimes, it’s easier to write a prescription than to have a hard conversation about stopping something.
Even worse, some of these drugs are sold over the counter. Benadryl is in sleep aids, allergy pills, and even some cold medicines. Older adults might not realize they’re taking multiple doses of the same dangerous ingredient.
Studies show that nearly 20% of older adults are taking at least one medication flagged by the Beers Criteria. And those who do are 30% more likely to be hospitalized for a drug-related problem.
What’s Changed in the 2023 Update?
The 2023 version didn’t just tweak a few names. It made big, clear changes based on new evidence.Antipsychotics are now strongly discouraged for people with dementia-even if they’re agitated or aggressive. These drugs don’t fix behavior. They just numb it. And they increase stroke risk and death. The AGS now says: try non-drug approaches first. If drugs are needed, use the lowest dose for the shortest time possible.
Benzodiazepines and similar sleep aids (like zolpidem) got a stronger warning. These drugs don’t just make you drowsy. They impair balance, slow reaction time, and increase fall risk by up to 50%. That’s not a small risk. It’s a life-changing one.
New criteria were added for drugs that increase fall risk-like certain blood pressure meds and diuretics. Even if they’re not on the “avoid” list, they’re now flagged as needing extra caution.
And for the first time, the panel included specific advice for people with reduced kidney function. Many drugs are cleared through the kidneys. As we age, kidney function drops-even if blood tests look “normal.” A dose that’s safe for a 50-year-old can build up to toxic levels in a 75-year-old.

How Is This Used in Real Life?
The Beers Criteria aren’t just sitting on a shelf. They’re built into hospital systems, nursing homes, and Medicare’s quality programs.Medicare Part D requires pharmacists to review medications for older adults. If someone’s on a Beers-listed drug, the pharmacist has to flag it. Nursing homes are scored on how often residents are on inappropriate meds. Hospitals use the criteria to check medication lists during discharge.
But here’s the catch: the AGS says these criteria are not rules. They’re guides.
“We don’t want doctors to feel punished,” says Todd Semla, one of the lead authors of the 2023 update. “Sometimes, a drug on the list is the best option for a patient. That’s why we emphasize individualization.”
For example, a person with severe arthritis and no other options might need an NSAID like ibuprofen-even though it’s on the caution list. The key is knowing the risk and monitoring closely. Or, a patient with chronic insomnia and no history of falls might still benefit from a low-dose sedative if non-drug options have failed.
That’s why the best use of the Beers Criteria is as a conversation starter-not a checklist.
What Should You Do If You or a Loved One Is on One of These Drugs?
Don’t stop taking anything on your own. But do ask these questions:- Is this medication still necessary? When was the last time we reviewed it?
- Are there safer alternatives? For example, can we try melatonin instead of a benzodiazepine for sleep?
- What are the risks if we keep taking it? What are the risks if we stop?
- Can we try reducing the dose first?
Ask for a full medication review. Many pharmacies offer free medication reviews for seniors. A geriatric pharmacist can look at everything you’re taking-prescription, over-the-counter, and supplements-and tell you what’s risky.
If you’re a caregiver, keep a written list of every drug, dose, and reason it was prescribed. Bring it to every appointment. Don’t assume the doctor remembers what was prescribed six months ago.
What About Other Tools Like STOPP-START?
There are other tools out there. STOPP-START looks at both inappropriate drugs and drugs that are missing-like not prescribing a statin for someone with heart disease.The Beers Criteria focus only on the bad ones. STOPP-START is broader. But Beers is simpler, more widely known, and built into U.S. healthcare systems. Most doctors and pharmacists know Beers. Fewer know STOPP-START.
Think of Beers as the alarm bell. STOPP-START as the full diagnostic. You don’t need both to start making safer choices. Beers is enough to begin.

The Bigger Picture: Medication Safety Is a Team Effort
Medication safety in older adults isn’t just about drugs. It’s about communication. It’s about time. It’s about respect.Too often, older adults are treated as passive recipients of care. Their preferences, values, and goals get ignored. A drug that reduces pain might also reduce independence. A pill that helps sleep might make someone too dizzy to walk to the bathroom. These trade-offs need to be discussed.
The Beers Criteria help bring those conversations into the open. They give patients and families the language to say: “This doesn’t feel right.”
And that’s the real power of the list. It doesn’t tell doctors what to do. It reminds them to think.
Final Thought: It’s Not About Perfect Prescribing. It’s About Safer Prescribing.
There’s no perfect drug for every older adult. But there are plenty of drugs that are clearly riskier than they need to be.The Beers Criteria don’t make prescribing easy. But they make it safer. And in a world where falls, confusion, and hospitalizations are common for seniors, that’s not just helpful-it’s essential.
If you’re over 65 and on multiple medications, ask for a review. If you’re caring for someone who is, don’t wait for a crisis. Start the conversation today.
Are all drugs on the Beers Criteria list banned for older adults?
No. The Beers Criteria list medications that carry higher risks than benefits for most older adults-but they’re not absolute bans. Some seniors may still need these drugs if other options don’t work. The key is careful monitoring and shared decision-making with a healthcare provider.
Can over-the-counter medicines be on the Beers Criteria list?
Yes. Many OTC drugs are included, especially antihistamines like diphenhydramine (Benadryl), sleep aids, and NSAIDs like ibuprofen. These are often overlooked because they’re available without a prescription, but they can be just as risky as prescription drugs in older adults.
How often are the Beers Criteria updated?
The American Geriatrics Society updates the Beers Criteria every 3 to 5 years. The most recent version was published in 2023, based on evidence reviewed from 2019 to 2022. Updates are made through a rigorous process involving expert panels and analysis of hundreds of clinical studies.
Is the Beers Criteria used outside the United States?
While the Beers Criteria were developed in the U.S., they’re used globally as a reference. Other countries have their own tools, like the STOPP-START criteria in Europe, but Beers remains one of the most cited and studied lists worldwide. Many international guidelines reference it when developing local standards.
Can the Beers Criteria help prevent falls in older adults?
Yes. Several drugs on the list-like benzodiazepines, antipsychotics, and certain blood pressure medications-are known to increase fall risk. By reducing or eliminating these, the risk of falls can drop significantly. In fact, studies show that deprescribing these drugs leads to fewer falls and fewer fractures in older adults.
Next Steps for Safer Medication Use
If you’re an older adult: make a list of every medication you take-including supplements and OTC drugs. Bring it to your next appointment. Ask: “Is this still right for me?”If you’re a caregiver: don’t wait for a hospital visit. Start the conversation now. Ask for a medication review. Use free resources like healthinaging.org to learn more.
If you’re a clinician: use the Beers Criteria as a starting point-not an endpoint. Talk to your patients. Listen. And remember: the goal isn’t to avoid all risk. It’s to make sure the benefit outweighs it.