Athlete AF Risk Calculator
Assess Your Risk Factors
Your Risk Assessment
Quick Takeaways
- Endurance training can trigger structural changes in the heart that raise AF risk.
- Typical warning signs include palpitations, shortness of breath, and unexplained fatigue.
- Diagnosis relies on ECG, Holter monitoring, and sometimes cardiac imaging.
- Treatment ranges from lifestyle tweaks to meds (beta‑blockers, anticoagulants) and catheter ablation.
- Regular check‑ups and balanced training are key to preventing episodes.
When a runner or cyclist feels their heart fluttering out of rhythm, it's easy to dismiss it as a harmless side effect of hard work. Yet for a growing number of high‑performance athletes, that flutter could be atrial fibrillation athletes - a genuine medical condition that demands attention. Below we break down what drives AF in active bodies, how to spot it, and what you can do to stay in the game.
What Is Atrial Fibrillation and Who Gets It?
Atrial Fibrillation is a rapid, irregular heart rhythm originating in the atria, the upper chambers of the heart. It causes electrical signals to fire chaotically, leading to an ineffective heartbeat and a higher risk of blood clots. While the condition is most common in people over 65, recent studies show a noticeable uptick among elite and recreational endurance athletes.
Athlete refers to anyone who engages in regular, intense physical training, especially in endurance sports like marathon running, cycling, rowing, and triathlon. These individuals push their cardiovascular system far beyond typical daily loads, creating a unique environment for heart rhythm disturbances.
Why Does AF Occur More Often in Endurance Athletes?
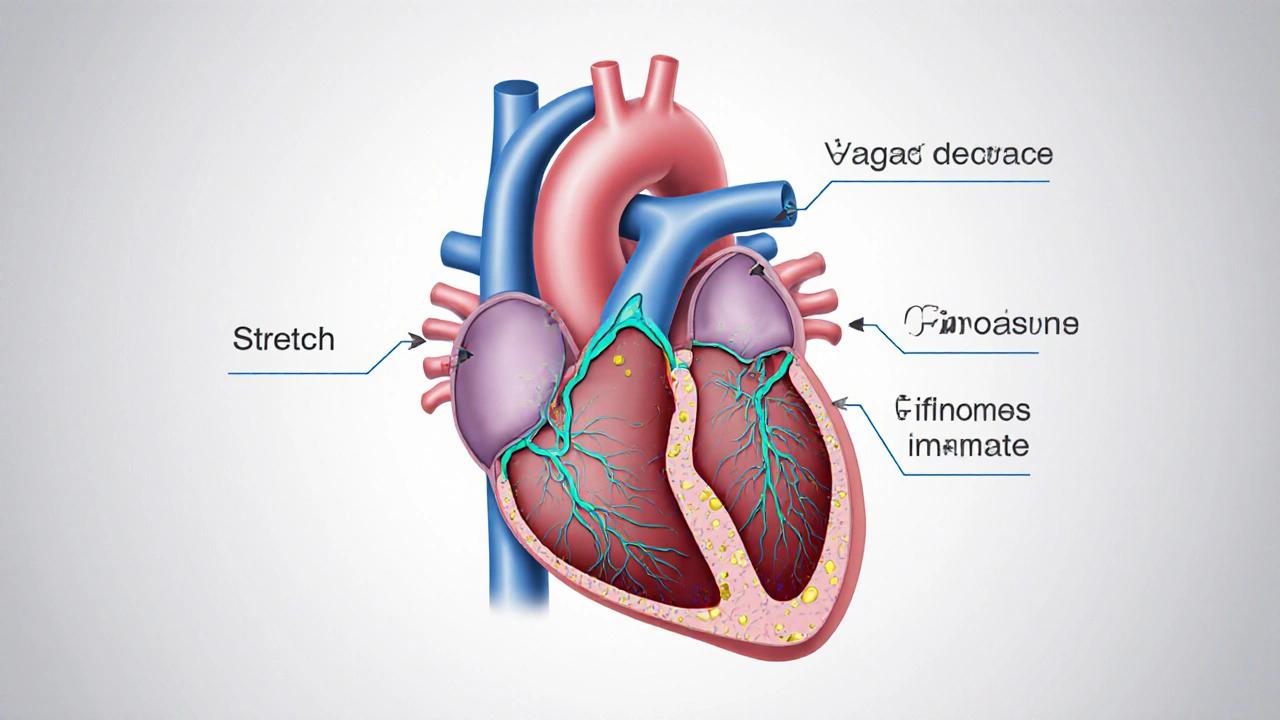
Three inter‑related mechanisms lie at the heart of the issue:
- Structural remodeling: Prolonged high‑volume training can cause the atria to enlarge, a condition known as atrial enlargement. This stretch alters the tissue’s electrical pathways, making them more prone to chaotic firing.
- Increased vagal tone: Vagal Tone represents the influence of the vagus nerve on heart rate, typically heightened in well‑trained athletes. While a strong vagal tone helps lower resting heart rate, it also predisposes the atria to premature beats that can trigger AF.
- Inflammation and fibrosis: Repeated bouts of intense exercise can lead to low‑grade inflammation. Over time, this may cause fibrotic scar tissue to develop in the atrial walls, disrupting the smooth flow of electrical impulses.
When these factors combine, the heart’s natural rhythm becomes fragile, especially during periods of high stress, dehydration, or electrolyte imbalance.
Spotting the Signs: Symptoms Athletes Shouldn't Ignore
AF can be silent, but many athletes notice one or more of the following during or after training:
- Palpitations - a rapid, fluttering sensation in the chest.
- Sudden shortness of breath that feels out of proportion to effort.
- Unexplained fatigue or a drop in performance despite unchanged training.
- Dizziness or near‑syncope, especially during high‑intensity intervals.
- Chest discomfort that isn’t typical muscle soreness.
Because these cues overlap with normal training fatigue, athletes often overlook them. If any symptom lasts longer than a few minutes or recurs regularly, it’s time to investigate.
How Is AF Diagnosed in an Athletic Population?
The diagnostic pathway mirrors that for the general public but is tailored to the athlete’s schedule and performance goals.
- Electrocardiogram (ECG): A quick, 10‑second snapshot of heart rhythm. In athletes, a resting ECG may appear normal even during an intermittent AF episode.
- Holter Monitor: A wearable device that records heart activity continuously for 24‑48hours, often revealing intermittent arrhythmias missed on a standard ECG.
- Event Recorder or Smart‑watch ECG: Modern wearables can capture a rhythm strip when the athlete feels a palpitation, providing valuable real‑time data.
- Echocardiogram: Uses ultrasound to assess atrial size, ventricular function, and any structural abnormalities such as valve disease.
- Cardiac MRI: In complex cases, MRI can quantify atrial fibrosis and guide treatment decisions.
Blood tests may also be ordered to rule out thyroid disorders, electrolyte imbalances, or inflammation that could aggravate AF.
Treatment Options: From Lifestyle Tweaks to Advanced Procedures
Choosing a treatment hinges on three factors: symptom severity, stroke risk, and the athlete’s performance goals.
1. Lifestyle and Training Adjustments
Before medication, most sports physicians recommend modifying training volume:
- Reduce ultra‑endurance sessions (>6hours) to moderate‑duration workouts.
- Incorporate regular strength‑training days to lower overall cardiac strain.
- Maintain optimal hydration and electrolyte balance, especially in hot climates.
- Prioritize sleep and stress‑reduction techniques (e.g., yoga, meditation).
These changes can lower vagal dominance and give the atria a chance to remodel back toward normal size.
2. Medication
When symptoms persist, doctors often prescribe one of two drug classes.
| Option | How It Works | Pros for Athletes | Cons / Risks |
|---|---|---|---|
| Beta‑Blocker Lowers heart rate and reduces arrhythmic triggers. | Blocks adrenaline effects, stabilizing heart rhythm. | Effective for rate control; inexpensive. | May blunt exercise performance; fatigue. |
| Anticoagulation Prevents clot formation, reducing stroke risk. | Inhibits clotting factors (e.g., warfarin, DOACs). | Critical for high stroke risk patients; minimal impact on performance. | Bleeding risk; regular monitoring for some agents. |
| Catheter Ablation Targets and destroys the tissue causing irregular signals. | Uses radiofrequency or cryotherapy to isolate pulmonary veins. | Potential cure; restores ability to train at high intensity. | Invasive; requires hospital stay; rare complications. |
Beta‑blockers are often the first line for athletes who need rate control without compromising clot protection. Anticoagulants become essential when the CHA₂DS₂‑VASc score (stroke risk calculator) exceeds 1, which can happen even in younger athletes with persistent AF.
3. Catheter Ablation - When to Consider It
For athletes who want to return to elite competition, catheter ablation is increasingly popular. Success rates exceed 80% for paroxysmal AF and 60‑70% for persistent forms. Recovery typically involves a brief hospital stay and a 2‑week limitation on high‑intensity training. Post‑procedure, many athletes report a return to pre‑AF performance levels.
4. Emerging Therapies
Research in 2024 highlighted the potential of low‑dose ranolazine and lifestyle‑focused digital health programs to lower AF burden in endurance athletes. While not yet standard care, these options may become part of a personalized treatment plan within the next few years.
Managing Long‑Term Risk and Prevention Strategies
Even after successful treatment, the underlying predisposition often remains. Here’s a checklist for athletes aiming to keep AF at bay:
- Schedule an annual cardiac evaluation, even if you feel fine.
- Keep training volume under 10hours per week for most endurance sports; vary intensity.
- Monitor resting heart rate; a sudden rise could signal overtraining.
- Stay on top of hydration and electrolyte intake, especially during long events.
- Use wearable ECG features to log any irregular beats and share the data with your doctor.
- Maintain a balanced diet rich in omega‑3 fatty acids, magnesium, and potassium.
- Avoid excessive alcohol and stimulant use (e.g., high‑dose caffeine) before competitions.
When to Seek Immediate Medical Attention
If you experience any of the following, call emergency services or visit an urgent care center:
- Chest pain lasting more than a few minutes.
- Severe shortness of breath at rest.
- Sudden loss of consciousness or near‑syncope.
- Rapid heart rate (>150bpm) that does not settle with rest.
These signals could indicate a more serious cardiac event, such as a stroke‑causing clot or a dangerous tachyarrhythmia.
Putting It All Together: A Practical Action Plan
Below is a step‑by‑step roadmap you can follow after suspecting AF:
- Stop the exercise session and note any symptoms.
- Use a wearable ECG or phone app to capture a rhythm strip.
- Contact your sports medicine physician within 24hours; share the rhythm strip.
- Undergo a 12‑lead ECG and a 24‑hour Holter (or event monitor) as advised.
- Discuss treatment options based on symptom severity and stroke risk.
- Implement recommended lifestyle changes alongside any prescribed meds.
- Schedule follow‑up testing in 3‑6months to assess response.
Sticking to this plan helps you regain confidence on the track or trail while safeguarding your long‑term heart health.

Frequently Asked Questions
Can occasional palpitations be normal for athletes?
Minor, brief palpitations are common, especially after very hard intervals. They’re usually benign if they stop within a minute and aren’t accompanied by dizziness or chest pain. Persistent or worsening episodes should be evaluated.
Do beta‑blockers always reduce performance?
Beta‑blockers can lower maximal heart rate, which may affect high‑intensity output. However, low‑dose formulations often allow athletes to maintain endurance performance while controlling rhythm. Discuss dosing with your cardiologist.
Is anticoagulation necessary for younger athletes?
If the CHA₂DS₂‑VASc score is 0‑1, some doctors may defer anticoagulation, especially if AF is infrequent. However, many opt for a direct‑acting oral anticoagulant (DOAC) because the bleeding risk is low compared with the potential stroke risk.
Can I return to full training after catheter ablation?
Most athletes resume moderate training within two weeks and high‑intensity work after 4‑6 weeks, provided follow‑up ECGs show stable rhythm. Your electrophysiologist will tailor the timeline.
Are there specific sports that carry higher AF risk?
Endurance disciplines that involve long, repetitive aerobic effort-marathon running, ultra‑cycling, cross‑country skiing, and rowing-have the strongest association. Sports with intermittent bursts (e.g., soccer) show a weaker link.


Shelby Wright
October 3, 2025 AT 08:15Well, look at this parade of medical jargon – it's like a circus of heartbeats, and I'm the ringleader screaming louder than the ambulance siren! You think athletes are just sprinters on a treadmill? No, they're basically cardio juggernauts dancing on the edge of arrhythmia, and the article barely scratches the surface. I love how it throws around terms like "atrial remodeling" like confetti at a wedding, but forget to mention the midnight cravings for caffeine and the existential dread that follows every race. Oh, and don't even get me started on the glorified "lifestyle tweaks" – as if swapping energy drinks for water will magically erase a decade of cardiac stress. So yeah, if you're planning to outrun your own heart, buckle up, because the rollercoaster's just begun.
Ellen Laird
October 4, 2025 AT 02:18Honestly, the prose in this piece is as pretentious as a wine‑snob at a craft‑brew fest. It attempts to sound scholarly while dropping misspellngs like "atrial enlargeement" and "vagal t0ne" – a delightful juxtaposition of highbrow and lowbrow. If you wanted a peer‑reviewed article, you might've consulted a cardiologist instead of a copy‑pasta generator.
rafaat pronoy
October 4, 2025 AT 20:21nice read, bro 😊 the info is solid and kinda reassuring. if you ever feel those weird flutter vibes, just grab your smartwatch and log it. keep it chill, stay hydrated, and enjoy the runs. peace.
sachin shinde
October 5, 2025 AT 14:25First, let us correct the sheer grammatical mishaps that pervade this article. The author erroneously writes "a higher risk" without a preceding article; the correct formulation is "a higher risk." Moreover, the phrase "low‑grade inflammation" should be hyphenated consistently throughout. Second, the content dangerously downplays the severity of atrial fibrillation in athletes, suggesting that "a few minutes of palpitations" are benign. This is not only misleading but also potentially life‑threatening. Third, the recommendation to "reduce ultra‑endurance sessions" is vague; specificity matters-one should limit continuous aerobic output beyond 10 hours per week, not merely "reduce" them. Fourth, the discussion of catheter ablation lacks a critical note on the need for post‑procedure anticoagulation in patients with CHA₂DS₂‑VASc scores ≥1. Fifth, the article falls short in addressing electrolyte monitoring, a cornerstone of arrhythmia prevention. Finally, the failure to cite primary research undermines its credibility. In summary, while the piece touches on relevant topics, it suffers from grammatical errors, insufficient clinical nuance, and a lack of scholarly rigor. Readers would benefit from a revised, evidence‑based version that adheres to both linguistic precision and medical accuracy.
Leon Wood
October 6, 2025 AT 08:28Hey everyone! Super pumped to see this thread – AF can feel scary, but remember, you’ve got the power to take charge of your heart health. Tiny tweaks like staying hydrated, pacing your long runs, and getting a quick check‑up can make a huge difference. Keep that positive mindset, trust your body, and don’t let fear hold you back from crushing those goals!
George Embaid
October 7, 2025 AT 02:31Great points, Leon! From a cultural perspective, many athletes worldwide overlook cardiac screening because of stigma. It’s essential to foster an inclusive environment where discussing heart health is as normal as talking about training splits. Let’s share resources across borders so everyone can stay safe while pursuing excellence.
Meg Mackenzie
October 7, 2025 AT 20:35Do you ever wonder why the "big pharma" and sports federations are so quick to push meds like beta‑blockers? It's like they're scared of a scenario where athletes run free without a pill‑in‑hand. The whole narrative feels orchestrated – they want you dependent, controlled, monitored. Trust your own body, not the hidden agendas.
Henry Kim
October 8, 2025 AT 14:38Thanks for sharing your concerns, Meg. It’s understandable to feel uneasy about pharmaceutical influence. Listening to your body, getting second opinions, and staying informed are practical steps you can take.
Neha Bharti
October 9, 2025 AT 08:41Training is a dialogue with the self. Balance intensity with recovery, and the heart will thank you.
Samantha Patrick
October 10, 2025 AT 02:45Great reminder, Neha! Also, make sure to check your electrolytes before long events – sodium and potassium are key. If you need a quick guide, just let me know.
Ryan Wilson
October 10, 2025 AT 20:48Everyone seems to be sugar‑coating this issue. In reality, if you keep ignoring the red flags, you’re basically cheering for a heart attack. It’s not a personal choice; it’s a public health crisis, and we all have a moral duty to speak up.
EDDY RODRIGUEZ
October 11, 2025 AT 14:51Ryan, you’re right – we can’t stay silent. But let’s channel that fire into action: schedule a cardiac screening, cut back on those endless ultra‑marathons for a month, and focus on strength work. You’ll come back stronger, and your heart will thank you.
Christopher Pichler
October 12, 2025 AT 08:55While the article provides a decent overview, its lack of depth on electrophysiological mapping is a glaring omission. For practitioners, understanding the nuances of pulmonary vein isolation techniques, including high‑power short‑duration ablation versus traditional settings, is crucial for optimizing outcomes. Moreover, the discussion fails to address the emerging role of AI‑driven predictive modeling in stratifying athletes' AF risk. Without incorporating these advanced concepts, the guide remains superficial and less useful for clinicians navigating complex cardiac cases in high‑performance athletes.
VARUN ELATTUVALAPPIL
October 13, 2025 AT 02:58Wow!!! This comment!!! Is!!! Overflowing!!! With!!! Punctuation!!! It!!! Seems!!! Like!!! A!!! Heartbeat!!! On!!! A!!! Stick!!!
April Conley
October 13, 2025 AT 21:01Let's be clear: education beats hype every time.