Alopecia areata isn’t just about losing hair-it’s about your immune system turning on your own hair follicles. One minute your scalp looks normal, the next, a coin-sized patch is completely bare. No itching, no scaling, no redness-just smooth, silent bald spots. It happens fast, often without warning, and it’s not caused by stress, poor diet, or bad hair care. This is an autoimmune condition, meaning your body’s defense system mistakenly attacks the hair follicles as if they’re invaders. And while it doesn’t threaten your life, it can shake your sense of self in ways few other skin conditions do.
How Alopecia Areata Actually Works
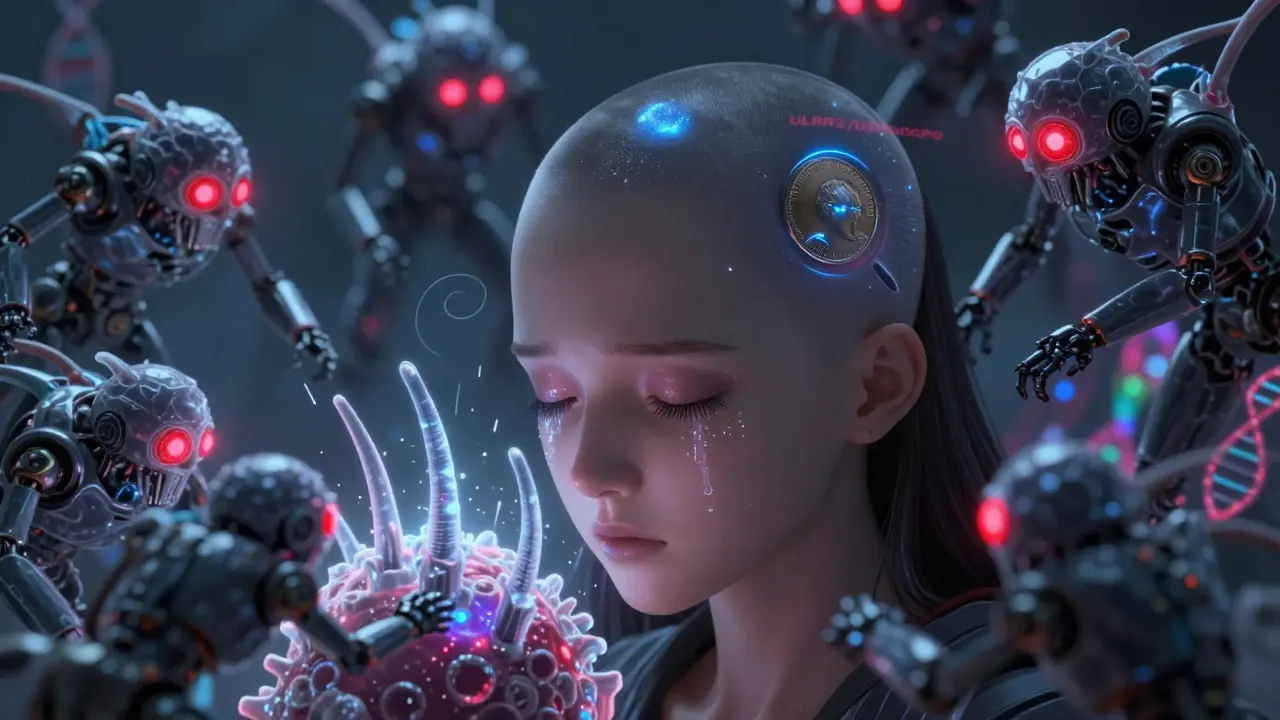
Your hair grows in cycles: anagen (growth), catagen (transition), and telogen (resting). In alopecia areata, the immune system disrupts this rhythm. Immune cells-mostly CD8+ T cells and natural killer cells-cluster around the base of the hair follicle like a swarm, forcing it to prematurely shut down. The follicle doesn’t die. It goes dormant. That’s why regrowth is possible, even after years of hair loss. The structure is still there, just silenced.
It’s not random. Research shows specific genes like ULBP3 and ULBP6 are involved, making some people more prone to this immune misfire. About half of all cases start before age 40, and men and women are affected equally. But women often report more severe emotional impact, likely because societal expectations around hair are stronger.
What you see on the scalp is just one version. Some people lose just one patch. Others lose all scalp hair (alopecia totalis). A few lose every hair on their body, including eyebrows, eyelashes, and even pubic hair (alopecia universalis). Then there’s ophiasis-a band of hair loss around the sides and back of the head-and diffuse alopecia, where hair thins all over without clear patches. Nail changes are common too: tiny dents (pitting), ridges, or rough surfaces. If you have these, it’s a clue your alopecia areata is more than skin-deep.
Why It’s So Different from Other Hair Loss
Most people think of hair loss as aging or hormones. Male pattern baldness? That’s driven by DHT, a hormone that slowly shrinks follicles over years. Telogen effluvium? That’s stress or illness pushing a bunch of hairs into the resting phase at once. Both are predictable. Both have patterns.
Alopecia areata is chaos. It doesn’t follow rules. One month you have a single patch. The next, three new ones appear. Or maybe the patch grows back, but a new one pops up on your eyebrow. That’s the hallmark: unpredictable, patchy, nonscarring. Unlike lichen planopilaris or frontal fibrosing alopecia-which destroy follicles permanently-alopecia areata leaves the door open. That’s why doctors say it’s one of the few hair loss conditions where hope isn’t just wishful thinking.
It’s also the second most common form of hair loss worldwide, after androgenetic alopecia. But unlike that condition, it’s not linked to testosterone or aging. It’s purely immune-driven. And that makes treatment trickier. You can’t just block a hormone. You have to calm a misfired immune system.
What Treatments Actually Work
There’s no cure. But there are treatments that help-some better than others, depending on how much hair you’ve lost.
Intralesional corticosteroid injections are the first-line treatment for patchy alopecia. A dermatologist injects a diluted steroid (like triamcinolone) directly into each bald patch every 4 to 6 weeks. It works by suppressing the local immune attack. About 60-67% of people with limited patches see regrowth within 3 months. But it’s painful. And it only works where you inject. If you have 20 patches, you’re in for a long road.
Topical steroids-like 0.1% betamethasone valerate lotion-are less effective but easier to use. You apply them daily. Results take 6 to 12 months. Only 25-30% of people get meaningful regrowth. It’s a slow burn, and many give up before seeing results.
Contact immunotherapy with DPCP is another option. You apply a chemical to your scalp weekly to trigger a controlled allergic reaction. The theory? Redirect your immune system away from the follicles. It works in 30-60% of cases, but it causes red, itchy, flaky skin. Not everyone can tolerate it. And again, it takes 6 to 12 months to know if it’s working.
JAK inhibitors changed everything in 2022. These are oral or topical drugs that block specific immune signals. Baricitinib (Olumiant) became the first FDA-approved treatment for severe alopecia areata in June 2022. In clinical trials, 35.6% of patients regained 80% of their scalp hair after 36 weeks. Ritlecitinib followed in June 2023, with 29.8% achieving the same result in just 24 weeks. These aren’t miracle cures. They don’t work for everyone. And they’re expensive-$10,000 to $15,000 a month in the U.S. Insurance often denies coverage unless you’ve tried everything else.
One patient from the Alopecia Areata Support Group described watching her hair grow back gray first, then slowly return to its natural color. “It was like seeing magic,” she said. But for others, the hair comes back, then falls out again after stopping the drug. Relapse rates hit 75% within a year of stopping JAK inhibitors. That’s the catch: you might need to stay on them long-term.

The Emotional Toll Nobody Talks About
Alopecia areata doesn’t kill you. But it can break you.
Studies show 30% of patients have moderate to severe anxiety. 28% meet the criteria for clinical depression. The National Institutes of Health says it has the highest quality-of-life burden of any skin disease-even worse than psoriasis and eczema. Why? Because hair is identity. It’s tied to youth, attractiveness, control. Losing it publicly-on the street, at work, in photos-feels like losing part of yourself.
One Reddit user with beard loss said: “After six months of injections, I got 40% regrowth. But the stress of waiting, the pain, the fear it wouldn’t work… it made me lose hair in new places. The treatment became part of the problem.”
Many avoid swimming, beaches, or even family gatherings. 42% of surveyed patients say they skip public water activities because they’re ashamed. That’s not vanity. That’s isolation.
Support groups matter. Not because they offer cures-but because they offer understanding. Talking to someone who knows what it’s like to wake up and find a bald spot on your eyebrow… that’s not something a dermatologist can replicate.
What Doesn’t Work (And Why People Waste Money)
There’s a market for miracle cures. Essential oils. Scalp massages. Supplements. Hair growth shampoos. Some people swear by them. But here’s the truth: there’s zero high-quality evidence that any of these reverse autoimmune hair loss.
Minoxidil (Rogaine) is often tried. It works for androgenetic alopecia. For alopecia areata? Studies show 0-15% efficacy in extensive cases. That’s not a treatment. That’s a placebo with a price tag.
And don’t fall for “natural immune boosters.” Your immune system isn’t weak-it’s confused. You don’t need to “boost” it. You need to calm it. Taking turmeric or zinc won’t stop CD8+ T cells from attacking your follicles.
Some clinics offer PRP (platelet-rich plasma) or low-level laser therapy. These might help with general thinning. But for true autoimmune alopecia? No solid data. They’re expensive. And they delay real treatment.

What’s Coming Next
The future isn’t just about more drugs. It’s about smarter ones.
Researchers at Columbia University are developing biomarker panels to predict who will respond to JAK inhibitors before they even start. Think of it like a blood test that says: “You have a 70% chance of responding to ritlecitinib.” That could save months of trial, error, and heartbreak.
Combination therapies are being tested too. Maybe a short course of steroids followed by a low-dose JAK inhibitor. Or topical JAK inhibitors paired with immunotherapy. The goal? Less side effects, lower cost, better long-term results.
The National Alopecia Areata Foundation projects a 50% reduction in disease burden by 2030. That doesn’t mean a cure. It means fewer people losing their hair. Fewer people feeling ashamed. More people getting effective help before it’s too late.
Right now, the best thing you can do is see a dermatologist who specializes in hair loss. Don’t wait for it to get worse. Don’t waste months on oils and shampoos. Get tested. Get a diagnosis. And know this: you’re not alone. Millions of people have walked this path. And science is catching up fast.
When to See a Doctor
You don’t need to wait for it to spread. If you notice:
- Sudden, smooth bald patches on your scalp, eyebrows, or beard
- Multiple patches appearing over weeks
- Nail pitting or ridges along with hair loss
- Scalp tingling or itching before hair falls out
Make an appointment. A dermatologist can confirm alopecia areata with a simple exam-or a scalp biopsy if needed. Early treatment gives you the best shot at regrowth. And it helps you avoid the emotional spiral that comes with uncertainty.
Is alopecia areata contagious?
No, alopecia areata is not contagious. It’s an autoimmune condition, meaning your immune system attacks your own hair follicles. You can’t catch it from someone else, and you can’t spread it through touch, sharing combs, or close contact.
Can alopecia areata be cured?
There’s no permanent cure yet. But many people experience full regrowth, sometimes without treatment. For others, treatments like JAK inhibitors can restore significant hair. The challenge is that hair loss often returns after stopping treatment. The goal now is long-term control, not just a one-time fix.
Do stress or diet cause alopecia areata?
Stress and diet don’t cause alopecia areata, but they can trigger flare-ups in people who are genetically prone. The root cause is immune dysfunction, not lifestyle. That’s why people who eat perfectly or meditate daily can still develop it-and why others with high stress never do.
How long does it take for hair to grow back?
It varies. About 80% of people with small patches regrow hair within a year, even without treatment. With treatment, regrowth can start in 2-3 months. But for extensive cases-like totalis or universalis-it can take a year or more. Hair often grows back fine and white at first, then regains color over time.
Are JAK inhibitors safe for long-term use?
JAK inhibitors like baricitinib and ritlecitinib are FDA-approved for severe alopecia areata, but they carry risks: increased chance of infection, blood clots, and certain cancers. They’re not for everyone. Doctors monitor blood counts and liver function regularly. They’re typically reserved for patients who haven’t responded to other treatments, and only after a full risk-benefit discussion.
Can children get alopecia areata?
Yes. About half of all cases start before age 40, and many begin in childhood. Children can develop patchy, total, or universal hair loss. Treatment options are more limited for kids-steroid injections and topical therapies are preferred. JAK inhibitors are being studied in younger patients but aren’t yet widely approved for those under 18.

wendy parrales fong
December 26, 2025 AT 03:35It’s wild how hair is tied to identity, you know? I lost a patch last year and suddenly felt like I was invisible in public. Not because of the bald spot-but because people looked away like it was rude to stare. No one talks about that part.
It’s not vanity. It’s grief. You’re mourning something you didn’t even realize you loved until it was gone.
Jeanette Jeffrey
December 27, 2025 AT 13:22Ugh. Another ‘feel-good’ post about autoimmune hair loss. Let’s be real-most people who post this stuff just want sympathy. JAK inhibitors cost $15k/month? Congrats, you’re rich enough to afford a luxury disease. Meanwhile, I’m paying rent with my last two paychecks.
Stop romanticizing suffering. It’s not a TED Talk. It’s a medical condition with shitty options.
Shreyash Gupta
December 28, 2025 AT 05:07Bro… I tried minoxidil for 8 months. Zero results. Then I started rubbing onion juice on my scalp. Like, actual onion. Smelled like a dumpster fire. But guess what? A tiny patch came back.
Science says it doesn’t work. My scalp says otherwise. 🤷♂️🧅
Dan Alatepe
December 29, 2025 AT 08:44Let me tell you something… I lost my beard. My whole damn beard. One morning, poof. Gone. Like someone erased it with an eraser. I cried in the shower. Then I shaved the rest off. Now I look like a monk who lost his religion.
But here’s the twist-I started dating again. People said I looked ‘mysterious.’ Turns out, bald doesn’t mean broken. It just means… different. And different is kinda hot. 😎
Angela Spagnolo
December 30, 2025 AT 12:51I… I didn’t know… about the nail pitting… I thought it was just… bad manicures… but last month… my dermatologist… looked at my fingers… and said… ‘That’s alopecia areata.’… I didn’t even… connect the dots… I’m so… confused… and… scared…
Is… is this… permanent…? I’m… just… trying… to… understand…
Sarah Holmes
December 30, 2025 AT 13:31How dare you call this ‘hopeful’? You’re selling false hope with JAK inhibitors and $15,000 monthly bills. This isn’t medicine-it’s corporate exploitation wrapped in emotional manipulation. People are being sold a dream they can’t afford while the pharmaceutical industry rakes in billions.
Real compassion would be universal healthcare. Not ‘you can regrow your hair if you’re lucky enough to have insurance.’
Michael Bond
December 31, 2025 AT 09:49My cousin had it. Regrew all her hair in 11 months. No treatment. Just time. So yeah-hope isn’t fake. It’s just unpredictable.
Matthew Ingersoll
January 1, 2026 AT 17:43In my village in rural India, we treat hair loss with neem oil and chants. No one knows what an autoimmune disorder is. But we know when someone is suffering. We sit with them. We don’t fix it. We just don’t look away.
Maybe the real treatment isn’t in a pill. Maybe it’s in presence.
carissa projo
January 2, 2026 AT 08:20I’ve been living with alopecia for 14 years. I’ve worn wigs. I’ve worn scarves. I’ve cried in parking lots. But here’s what no one tells you-when you stop fighting your reflection, something shifts.
My hair came back gray at first. Then it turned brown. Then it turned curly. I didn’t recognize myself. But I learned to love the new version. Not because I was ‘strong.’ But because I had to.
You’re not broken. You’re becoming.
And if you need to scream into a pillow today? Do it. Then tomorrow? Try a new hat. Just for fun.
josue robert figueroa salazar
January 3, 2026 AT 19:44JAK inhibitors are a scam. I tried them. Hair came back. Then fell out. Then came back gray. Then fell out again. Now I’m on disability. My insurance dropped me. The company made billions. I made a bald head.
Don’t waste your money. Or your hope.