Potassium Intake Calculator for ACE Inhibitor Patients
Enter the foods you've eaten today. The calculator shows your total potassium intake and whether it's safe based on your kidney function. For patients with eGFR below 45, aim for under 2,000 mg/day.
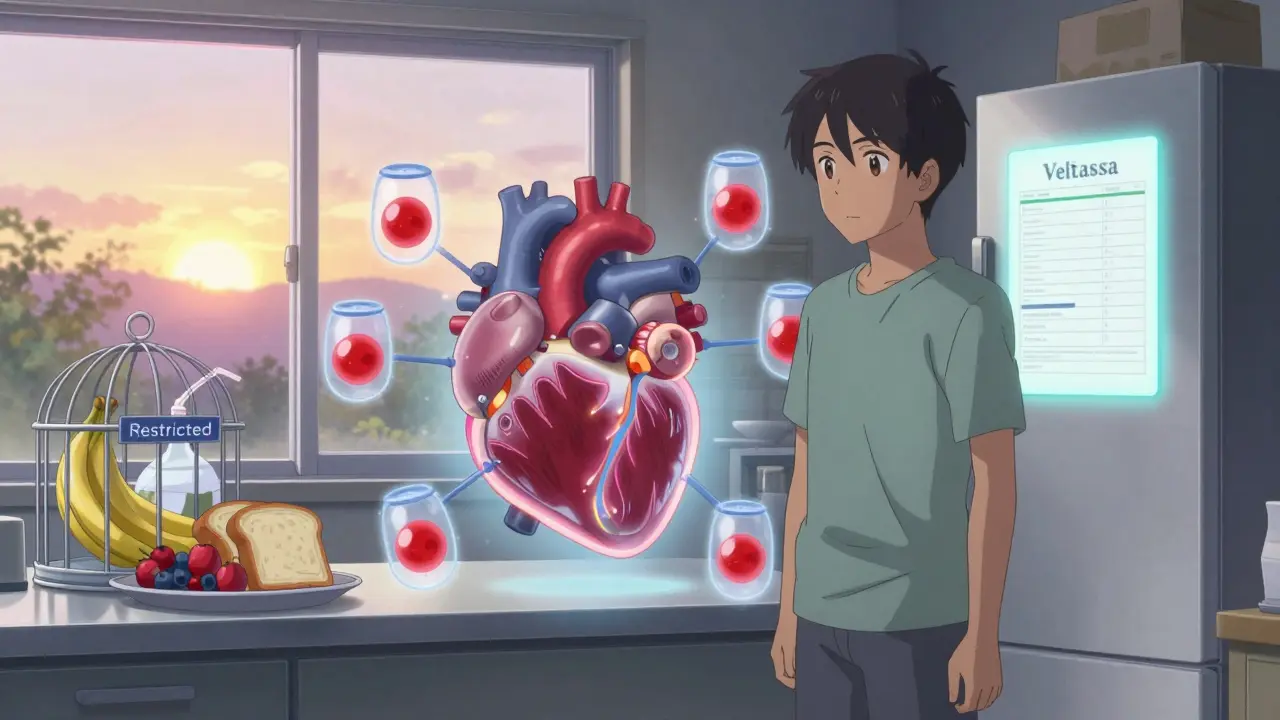
Why ACE Inhibitors Can Raise Your Potassium Levels
ACE inhibitors are common medications for high blood pressure, heart failure, and kidney disease. They work by relaxing blood vessels and reducing strain on the heart. But there’s a hidden side effect many patients don’t know about: they can cause your potassium levels to climb dangerously high. This condition is called hyperkalemia, and it can lead to irregular heartbeats, muscle weakness, or even cardiac arrest if left unchecked.
The reason? ACE inhibitors block a hormone system in your body called RAAS. One key part of that system is aldosterone, a hormone that tells your kidneys to flush out extra potassium. When ACE inhibitors shut down aldosterone, potassium builds up instead of leaving your body. Studies show that between 10% and 24% of people taking these drugs develop high potassium - and the risk jumps even higher if you have kidney disease, diabetes, or are over 75.
Who’s at the Highest Risk?
Not everyone on ACE inhibitors needs to worry equally. Certain groups are far more likely to develop hyperkalemia:
- People with chronic kidney disease (eGFR below 60)
- Diabetics, especially those with protein in their urine
- Patients over 75 years old
- Those already taking other drugs that raise potassium, like spironolactone or trimethoprim
- Heart failure patients with advanced symptoms (NYHA Class III or IV)
A 2021 study found diabetic patients on ACE inhibitors had a 47% higher chance of developing high potassium than non-diabetics. And if you have both diabetes and kidney disease, your risk multiplies. That’s why doctors check your blood potassium and kidney function before starting the drug - and again within two weeks.
Which Foods Are Dangerously High in Potassium?
While your kidneys handle most of your potassium balance, what you eat matters - especially if your kidneys are already struggling. The National Kidney Foundation recommends limiting potassium to under 2,000 mg per day if your eGFR is below 45. Here are common foods that can push your levels too high:
- Bananas (422 mg per medium fruit)
- Oranges and orange juice (237 mg per medium fruit)
- Baked potatoes (926 mg per medium potato)
- Spinach (839 mg per cup cooked)
- Avocados (708 mg per cup)
- Tomatoes and tomato sauce (292 mg per medium tomato)
- Sweet potatoes (542 mg per medium potato)
- Coconut water (1,150 mg per 16 oz)
- White beans and lentils (over 600 mg per half cup)
- Many protein powders and sports drinks (check labels - some contain added potassium)
It’s not just about eating a few bananas. It’s about the total daily load. One person might eat a banana, a baked potato, spinach salad, and a glass of coconut water - and unknowingly hit 2,500 mg of potassium in one meal. That’s enough to trigger a spike in someone with reduced kidney function.

How to Eat Smarter Without Giving Up Healthy Foods
You don’t have to eliminate all healthy foods. You just need to be smarter about how you prepare and portion them.
- Leach vegetables: Cut potatoes, carrots, and beets into small pieces, soak them in warm water for 2+ hours, then rinse and boil them in fresh water. This removes up to 50% of the potassium.
- Choose lower-potassium fruits: Apples, berries, grapes, pineapple, and watermelon are safer choices.
- Swap out high-potassium staples: Use white rice instead of brown, regular pasta instead of whole grain, and white bread instead of whole wheat.
- Avoid salt substitutes: Many contain potassium chloride - a hidden source of potassium that can be deadly when combined with ACE inhibitors.
- Read labels: Check ingredient lists for potassium chloride, potassium phosphate, or potassium citrate - common additives in processed foods and protein shakes.
One patient on Reddit shared how she avoided a hospital visit after realizing her daily protein shake contained 1,200 mg of potassium. She switched to a brand without added minerals and hasn’t had a spike since.
Monitoring and Testing: What Your Doctor Wants You to Know
Your doctor isn’t just checking your blood pressure. They’re watching your potassium and kidney numbers closely. Here’s the standard testing schedule:
- Before starting an ACE inhibitor: Baseline blood test for potassium and creatinine
- 7-14 days after starting: First follow-up test
- After any dose increase: Test within a week
- Every 4 months: Routine monitoring, even if you feel fine
A slight rise in creatinine (up to 30%) is normal and doesn’t mean you need to stop the drug. But if your potassium climbs above 5.5 mmol/L, your doctor will likely adjust your diet, reduce your dose, or add a potassium binder like Lokelma or Veltassa.
These newer binders are game-changers. Clinical trials show they cut the number of people forced to quit ACE inhibitors by 41%. They work by trapping potassium in your gut so it leaves your body in stool instead of building up in your blood.
What to Do If You’ve Already Had a High Potassium Episode
If you’ve ever had a potassium level above 5.5 mmol/L, you’re at higher risk for another one. Here’s what you should do:
- Meet with a renal dietitian - not just any nutritionist. They know exactly which foods to avoid and how to make meals safe.
- Use a potassium-tracking app like Renal Diet Helper. It lets you scan foods and track daily intake.
- Keep a laminated food chart on your fridge. Many hospitals give these out for free.
- Don’t skip your blood tests, even if you feel fine. High potassium often has no symptoms until it’s too late.
- Talk to your doctor before starting any new supplement, including herbal teas or magnesium.
A 2022 study found that patients who got both written materials and in-person counseling from a dietitian were 42% more likely to stick to their potassium limits than those who only got handouts.
When to Call Your Doctor Immediately
High potassium doesn’t always cause obvious symptoms. But if you notice any of these, get help right away:
- Heart palpitations or fluttering in your chest
- Unexplained muscle weakness or numbness
- Nausea or vomiting without a clear cause
- Feeling unusually tired or dizzy
These could be signs your potassium is dangerously high. Don’t wait. Call your doctor or go to urgent care. A simple blood test can confirm it - and if needed, emergency treatment like IV calcium or dialysis can quickly bring levels down.
The Bottom Line: You Can Stay Safe Without Stopping Your Medicine
ACE inhibitors save lives. They reduce heart attacks, slow kidney damage, and help people live longer. But they’re not risk-free. The key is managing the risk - not avoiding the drug.
With proper monitoring, smart eating, and the right tools, most people can take ACE inhibitors safely for years. The goal isn’t perfection. It’s awareness. Know your numbers. Know your foods. Know your limits.
And if you’re unsure about what to eat, ask for help. A renal dietitian can make a bigger difference than any pill.
Can I still eat bananas if I’m on an ACE inhibitor?
It depends on your kidney function and current potassium levels. If your eGFR is below 45 or your potassium has ever been above 5.0 mmol/L, it’s safest to avoid bananas or limit them to half a fruit once a week. For people with healthy kidneys and normal potassium, one banana a day is usually fine. Always check with your doctor or dietitian before making changes.
Do all ACE inhibitors raise potassium the same amount?
Yes - the effect on potassium is similar across all ACE inhibitors like lisinopril, enalapril, and ramipril. The risk comes from how the drug works, not which one you take. However, higher doses increase the risk. That’s why doctors start low and go slow.
Is it safe to use salt substitutes on an ACE inhibitor?
No. Most salt substitutes replace sodium chloride with potassium chloride. That means you’re adding extra potassium directly into your diet - exactly what your body can’t handle well on ACE inhibitors. Even one teaspoon can add 800 mg of potassium. Stick to regular salt in moderation, or use herbs and spices instead.
Can I stop eating potassium-rich foods forever?
Not necessarily. Many people can gradually increase their potassium intake once their kidney function stabilizes and their levels are consistently normal. But this should only be done under medical supervision. A dietitian can help you find a balance between safety and nutrition.
What if I forget to take my blood test?
Skipping tests is risky. High potassium often has no symptoms until it’s life-threatening. Many patients think they’re fine because they feel okay - but their potassium could be rising silently. Set phone reminders. Ask your pharmacy to call you before your next test. Your doctor needs this data to keep you safe.
Are there any new treatments to help manage potassium levels?
Yes. Two new medications - patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) - bind potassium in your gut and remove it through stool. They’re approved for people on ACE inhibitors who keep developing high potassium. These drugs let patients stay on life-saving heart and kidney medications without having to stop them. They’re not for everyone, but they’ve changed the game for many.


rahulkumar maurya
February 4, 2026 AT 07:47Let me be perfectly clear: if you're on an ACE inhibitor and still eating bananas like they're candy, you're not just ignorant-you're actively endangering yourself. This isn't 'diet advice,' it's basic physiology. The RAAS system isn't a suggestion; it's a biological firewall. Ignoring it because 'I feel fine' is the exact mindset that lands people in the ICU with arrhythmias. You want longevity? Then respect the science, not your cravings.
Demetria Morris
February 6, 2026 AT 05:22I've been on lisinopril for 8 years. I swapped bananas for apples, stopped using salt substitute (who knew that was a trap?), and now my potassium stays at 4.1. It's not hard. It's just… inconvenient for people who think their taste buds are more important than their heart.
pradnya paramita
February 7, 2026 AT 02:08For those managing hyperkalemia on ACEi, it's critical to understand that potassium homeostasis is a triad: renal excretion, transcellular shifts, and dietary intake. When eGFR falls below 45 mL/min/1.73m², aldosterone suppression from ACEi significantly impairs distal nephron K⁺ secretion. Leaching vegetables reduces K⁺ content by 30–50% via diffusion into aqueous medium-this is supported by KDIGO guidelines. Also, avoid potassium-containing additives like potassium chloride, potassium phosphate, and potassium citrate in processed foods. Consider Veltassa if dietary management fails-its K⁺ binding capacity exceeds 30 mEq/day with minimal GI side effects.
Jamillah Rodriguez
February 7, 2026 AT 23:25OK but like… why does EVERYTHING have potassium now?? 🥲 I tried to make a smoothie and my protein powder had more K than a whole banana. I’m just trying to get through the day without a heart attack 😭
Susheel Sharma
February 8, 2026 AT 00:11Let’s be real: the medical-industrial complex profits from fear. ACE inhibitors are overprescribed. The potassium panic? A distraction. People die from statins, not from eating a sweet potato. Your doctor wants you scared so you’ll keep taking pills and never question the protocol. You think they care about your kidneys? They care about their bonuses. Read the FDA adverse event reports. It’s not the food-it’s the drug.
Joseph Cooksey
February 8, 2026 AT 12:16Look, I’ve been a nephrologist for 27 years, and I’ve seen more patients die from ignoring potassium than from the ACE inhibitors themselves. The problem isn’t the medication-it’s the cultural delusion that ‘natural’ means ‘safe.’ Avocados are not a virtue. Coconut water is not a health elixir. And if you think your ‘clean eating’ lifestyle overrides the biochemistry of your failing kidneys, you’re not just wrong-you’re a walking time bomb. The data is irrefutable: hyperkalemia mortality rises exponentially above 5.5 mmol/L. You don’t get to opt out of physiology because you dislike the taste of white rice. This isn’t a lifestyle blog. It’s a survival manual.
Justin Fauth
February 8, 2026 AT 23:15Y’all are acting like this is some new conspiracy. Back in my day, we just ate what we were given and didn’t whine about potassium. If you can’t handle a little potassium, maybe you shouldn’t be on meds meant for people with real problems. This country’s gone soft. We used to just take our pills and eat our food. Now we need apps, charts, dietitians, and leaching instructions for potatoes. What’s next? A permit to breathe?
Meenal Khurana
February 9, 2026 AT 00:28Leaching potatoes works. I do it every Sunday. Simple. Effective.
Shelby Price
February 9, 2026 AT 09:30So… if I eat one banana a week and avoid the rest, am I okay? Or is it the cumulative effect? I’m confused 😅
Jesse Naidoo
February 9, 2026 AT 10:55Wait, so you’re saying I can’t have my avocado toast anymore? But it’s my morning ritual. I feel like you’re taking away my joy. I’m not asking for much-just one slice… can’t we just… compromise? 🥺
Sherman Lee
February 10, 2026 AT 21:26Ever wonder why potassium levels are suddenly a big deal? Big Pharma bought the FDA. They want you dependent on Veltassa-$1,200/month pills-so you never stop taking ACE inhibitors. The real cause of hyperkalemia? Glyphosate in your food. It damages your adrenal glands. Read the papers from the 1990s. They buried this. They don’t want you to know.
Lorena Druetta
February 11, 2026 AT 00:47To everyone struggling with this: you are not alone. This journey is hard, but you are strong. Every small choice-choosing an apple over a banana, skipping the salt substitute, setting that blood test reminder-you are choosing life. I believe in you. Keep going. One day at a time. 💪❤️
Zachary French
February 11, 2026 AT 23:26Okay so I just found out my ‘healthy’ granola bar had potassium citrate in it. Like… WHO PUT THAT THERE?? I’m not even sick and I’m already at risk?? This is a trap. I feel like I’m living in a dystopia where even my oatmeal is trying to kill me. 😭
Coy Huffman
February 13, 2026 AT 15:02I think we’re missing the bigger picture here. The real issue isn’t potassium-it’s how disconnected we’ve become from our bodies. We treat food like data points and medicine like a magic bullet. Maybe the solution isn’t just leaching potatoes, but relearning how to listen. My potassium stabilized when I stopped obsessing over numbers and started eating slowly, mindfully, with my family. Not because I followed a list-but because I remembered what food is for.
Nathan King
February 14, 2026 AT 13:49It is imperative to underscore that the clinical efficacy of ACE inhibitors in reducing all-cause mortality in patients with heart failure and diabetic nephropathy is unequivocally established in randomized controlled trials with median follow-up exceeding five years. The risk of hyperkalemia, while statistically significant, remains numerically low in the context of overall benefit. To abandon these agents on the basis of dietary mismanagement or non-adherence to monitoring protocols constitutes a clinically indefensible therapeutic regression. The onus is on the patient to engage in evidence-based behavioral modification-not on clinicians to compromise pharmacologic efficacy.